J AM COLL RADIOL:你听说过同步虚拟放射学会诊吗?其在动脉粥样硬化疾病初级保健中的应用
2022-07-14 shaosai MedSci原创
现阶段,在心血管疾病的初级预防中利用医学影像是一个特别有前途的新兴战略。
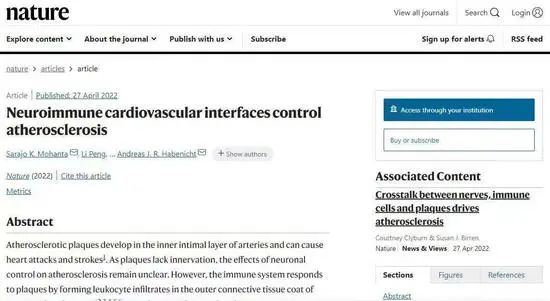
尽管世界卫生组织预计约90%的动脉粥样硬化性心血管疾病(CVD)可以在50岁之前通过减少危险因素来预防,但CVD的预防仍然是临床上所面临尚无艰巨问题之一。目前医疗机构使用的基于流行病学的工具可能低估了某些种族/民族人群或具有类似合并风险因素的队列的CVD风险,对准确量化风险和随后确定适当的临床管理建议构成挑战。因此需要有新的策略来更准确地估计CVD风险并影响临床预后。
现阶段,在心血管疾病的初级预防中利用医学影像是一个特别有前途的新兴战略。尽管放射科医生在评估动脉粥样硬化疾病的程度方面发挥积极作用,但他们可能很少直接与患者直接交流影像学结果。
基于转诊的放射科患者咨询门诊代表了一种直接向患者传达心血管疾病风险的新策略。鉴于对放射科医生日常工作流程的干扰,包括按需放射科会诊在内的其他模式难以大规模实施。临床上引入的护理点同步虚拟放射学会诊解决了这些局限性,这是一种新兴的护理模式,放射科医生可通过电话或视频会议与病人和他们的医疗机构同时沟通。
然而,涉及放射科医生和初级保健医生的护理点同步虚拟访问对患者态度和对动脉粥样硬化疾病的看法的影响还没有被评估。
近日,发表在J AM COLL RADIOL杂志的一项研究探讨了对于CT影像上有动脉粥样硬化钙化的患者来说,如果参与同步护理点虚拟放射学咨询是否可以更好地了解自身的疾病程度,并实现医患心血管危险因素的共同管理。

本项研究中将纳入了107名年龄和性别匹配的患被分配到对照组(n = 62)和干预组(n = 45),纳入标准如下:
(1)年龄大于45岁,
(2)有主治医生(PCP)会诊,
(3)近期胸部或腹部CT显示有动脉硬化钙化。在干预组中,与转诊的初级保健医生和患者进行虚拟实时放射学咨询,审查CT图像的重点是血管动脉粥样硬化的程度。对照组的病人遵循目前的标准,由初级保健医生讨论相关的影像学结果。
干预组的31名患者和对照组的31名患者完成了研究(对照组:64.5%为女性;平均年龄68岁;干预组:67.7%为女性;平均年龄68岁)。67.7%为女性;平均年龄为67岁)。干预组的所有患者都对影像学结果进行了讨论(与初级保健医生的讨论和与放射科医生的虚拟咨询),对照组有45%(仅与初级保健医生讨论;P < .001)。干预组的所有患者都表示看到或讨论他们的图像提高了他们对自己疾病的理解,而对照组有85%的患者由此感受(P=0.04)。在干预组中,31名患者中有10名(32.2%)在离开就诊时改变了他汀类药物或降压药的处方,而对照组中31名患者中只有4名(13%)(P = .04)。
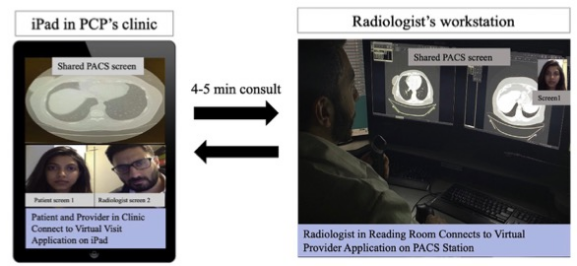
图 虚拟放射学咨询视频会议屏幕示例。放射科医生与医疗机构和病人实时审查研究。病人和主治医生(PCP)使用加密iPad上的虚拟访问应用程序与医疗机构诊所的放射科医生连接,该软件符合HIPAA标准。通过屏幕共享和视频会议,病人和初级保健医生可以在4-5分钟的虚拟放射学会诊中与放射科医生一起审查病人的放射图像
本项概念验证的试点研究评估了护理点同步虚拟放射学咨询对初级保健机构中以患者为中心的心血管危险因素管理的附加价值。本研究结果表明,与放射科医生的实时会诊可以提高患者对其健康状况的理解,并影响动脉硬化疾病的医疗管理。虚拟放射科会诊可通过提供更多个性化的放射科护理,并在以病人为中心的实践模式中促进坚持减少危险因素和预防疾病,从而推进放射科在护理服务中的价值。
原文出处:
John C Panagides,Nikhita Nambiar,Garrett Chinn,et al.Point-of-Care Synchronous Virtual Radiology Consultations for Atherosclerotic Disease in Primary Care: A Cluster-Randomized Study.DOI:10.1016/j.jacr.2021.10.013.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#Coll#
41
#初级保健#
47
#粥样硬化#
61
#会诊#
47
#放射学#
36