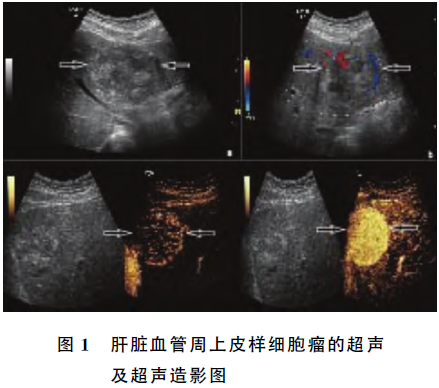
超声造影及增强CT诊断肝脏血管周上皮样肿瘤1例
2019-03-12 严玺德 王振兴 李发斌 中国超声医学杂志
患者女,49岁,汉族,已婚,农民。以3d前右下肢出现大片状红斑到我院皮肤科就诊收住入院。体格检查:无明显异常。实验室检查:肿瘤标记物CA72413.6U/ml,其余阴性。超声检查:肝左叶见大小约61mm×56mm实性略高回声占位,边界清晰,内部回声不均匀,CDFI:肿块周边及内部见较丰富血流信号。超声造影:造影剂注入肿块后9s呈环状且向心性轮辐样高增强,10s迅速强化,30s逐渐消退,肿块边界清晰
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#增强CT#
41
学习学习学习
57
#超声造影#
43
#造影#
30
#上皮样#
44