JHLT:肝脏的磁共振舒张测量可作为无创评估肺动脉高压右心衰竭的方法
2021-10-26 刘少飞 MedSci原创
肺动脉高压(PH)患者的右心衰竭(RHF)表现为右心房(RA)压力升高。肺动脉高压的右心衰竭在磁共振肝脏的评估具有更大的价值。
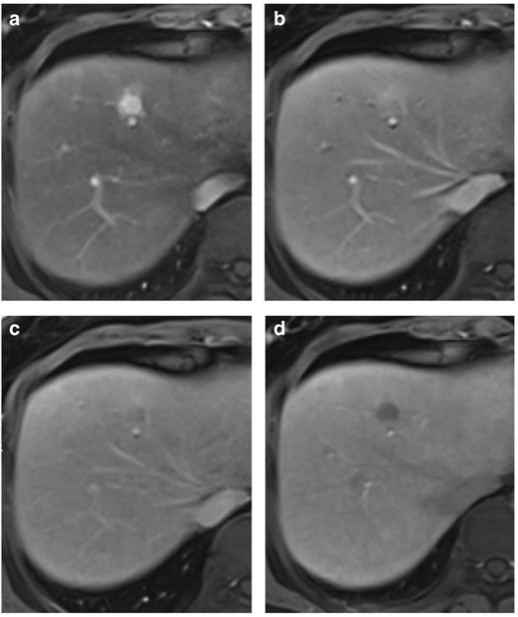
众所周知,肺动脉高压(PH)患者的右心衰竭(RHF)表现为右心房(RA)压力升高。该研究假设在心血管磁共振 (CMR) 下测量的肝脏舒张时间可用于无创评估右侧充盈压力的增加。
研究人群:
对于当前的研究,从 CMR 数据库中纳入了 45 名接受右心导管插入术的患者队列。37 名患者符合PH的诊断,而8名患者已知患有慢性血栓栓塞性肺病。在CMR检查的 48 小时内采集了右心导管插入术以及血液样本。与 40 名 CMR 结果对照受试者进行了比较。在心脏图上测量了天然 T1、T2 和细胞外体积 (ECV) 肝脏值。
研究结果:
RA 压力增加(即≥8 mm Hg)(n = 19,RA+ 组)的患者表现出更高的 NT-proBNP 和 CRP 值,更低的 LVEF、MAPSE 值,更大的心房大小,以及更高的心肌固有 T1 和 T2 值 RA 压力正常的患者(RA 组,n = 26)。RA+ 患者的肝脏 T1、T2 和 ECV 显着高于 RA- 患者和对照组,即 T1:684 ± 129 ms vs 563 ± 72 ms 和 540 ± 34 ms; T2:60 ± 10 ms vs 49 ± 6 ms 和 46 ± 4 ms; ECV:36 ± 8% 与 29 ± 4% 和 30 ± 3%。发现肝脏 T1、T2 和 ECV 与 RA 压力之间呈正相关,即 r2 分别为 0.61、0.82 和 0.58(p < 0.001)。描述 RA 压力增加的 ROC 分析显示,肝脏 T1、T2、NT-proNBP 和 γ-谷氨酰转肽酶的 AUC 分别为 0.847、0.904、0.816 和 0.645。在评估 T1/T2/ECV 肝脏值时发现观察者内部和观察者间的一致性极佳。
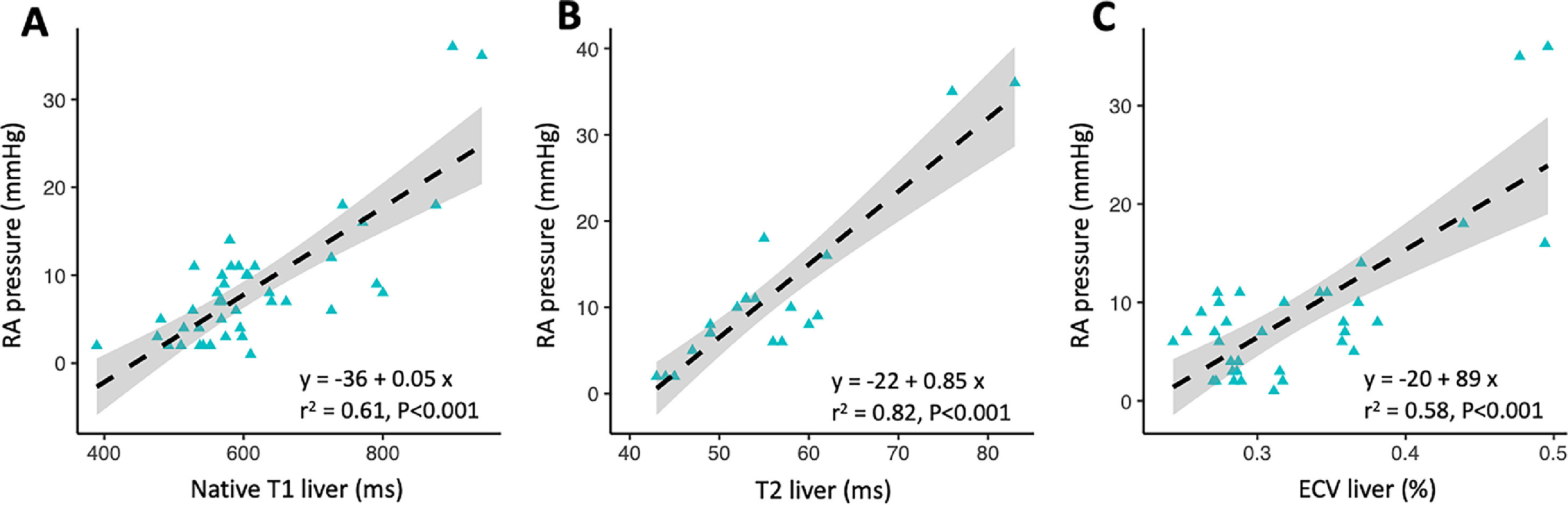
启示:目前的研究提供了令人信服的证据,表明作为综合 CMR 检查的一部分,肝脏舒张测定法可以通过检测和量化由于 CVP 升高引起的被动肝充血来实现 PH 患者的表型特征。事实上,我们发现天然肝脏 T1 或 T2 弛豫时间或 ECV 与有创测量的 RA 压力之间存在良好的相关性。值得注意的是,天然肝脏 T1 和 T2 值的诊断准确性并不逊于反映充血性心脏的生物标志物。
参考文献:
Bogaert J, Claessen G, Dresselaers T, Masci PG, Belge C, Delcroix M, Symons R. Magnetic resonance relaxometry of the liver - a new imaging biomarker to assess right heart failure in pulmonary hypertension. J Heart Lung Transplant. 2021 Sep 16:S1053-2498(21)02492-X. doi: 10.1016/j.healun.2021.09.005. Epub ahead of print. PMID: 34686407.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#动脉高压#
43
#右心衰竭#
51
#右心衰#
43
#心衰竭#
44
#磁共振#
38