J Sex Med:性功能障碍的阅读治疗:系统性回顾和元分析
2021-04-18 AlexYang MedSci原创
最近,有研究人员评估了阅读疗法治疗性功能障碍的疗效,并与不进行治疗以及其他干预措施进行了比较。
最近,有研究人员评估了阅读疗法治疗性功能障碍的疗效,并与不进行治疗以及其他干预措施进行了比较。

研究人员在MEDLINE, EMBASE和PsycINFO中搜索了1970年到2020年1月的相关文献。 选择标准是随机对照试验,评价了辅助或非辅助的阅读疗法与不治疗(等待名单或安慰剂)或其他心理干预相比治疗所有类型的性功能障碍的情况。阅读疗法是一种心理治疗,由患有性功能障碍的个人或夫妇使用。
研究共有15项随机对照试验,1113名参与者(781名女性;332名男性)符合纳入标准。研究结果表明,与不治疗相比,非辅助的阅读治疗使更大比例的女性参与者报告性功能障碍得到缓解,并且治疗参与者的性满意度更高(包括女性和男性参与者)。与未治疗相比,辅助阅读治疗对女性性功能有明显的积极作用;而对男性性功能没有影响。非辅助和辅助阅读治疗的结果与其他干预类型的结果在所有结果上都没有差异。整个来讲,考虑到流失率,研究条件之间没有发现差异。所有结果的证据的确定性为非常低。
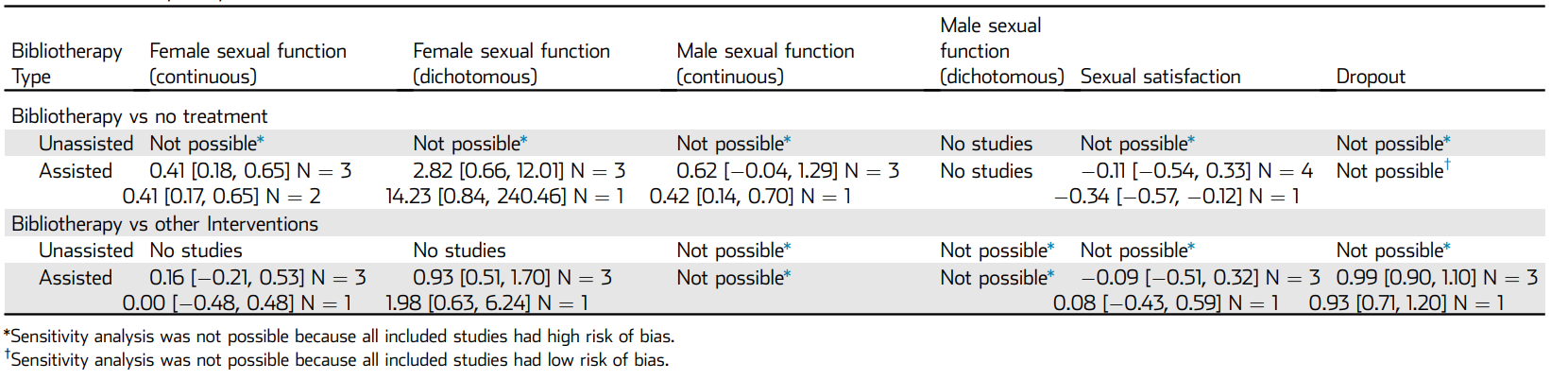
敏感性分析
最后,研究人员指出,有迹象表明,阅读疗法对性功能障碍有积极作用。在各项研究中发现女性的效果比男性更显著。然而,由于研究设计的局限性和研究结果的不精确性,研究人员无法对性功能障碍采用阅读疗法得出确切的结论。因此,需要更多高质量和更大规模的试验。另外,应定义未来研究的相关结果衡量标准以及统一的分级系统来衡量这些终点。此外,今后的研究应报告治疗的可接受性和依从性情况。
原始出处:
Jacques J D M van Lankveld , Fleur T van de Wetering , Kevan Wylie et al. Bibliotherapy for Sexual Dysfunctions: A Systematic Review and Meta-Analysis. J Sex Med. Mar 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#元分析#
40
#系统性#
39
学习学习
52
#功能障碍#
32
#Med#
39