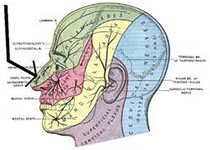
CLIN CANCER RES:Tim-3+ Treg细胞在头颈部肿瘤患者中发挥抑制作用
2018-09-29 MedSci MedSci原创
调节性T(Treg)细胞是肿瘤浸润淋巴细胞(TIL)中的重要抑制细胞。Treg细胞表达免疫检查点受体PD-1,既往报道表达PD-1的Treg为抑制功能较低的"耗竭性"Treg。T细胞免疫球蛋白粘蛋白(Tim)-3是Th1免疫的负性调节因子,大量TIL Tregs均有表达,但Tim-3 + Tregs的功能目前仍不清楚。CLIN CANCER RES近期发表了一篇文章研究这一问题。
原始出处:
Zhuqing Liu, Elizabeth L,et al. CDK9 Inhibitor Novel
Effector Phenotype of Tim-3+ Regulatory T Cells Leads to Enhanced Suppressive
Function in Head and Neck Cancer Patients.CLIN CANCER RES.September 2018 doi: 10.1158/1078-0432.CCR-17-1350
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#TIM-3#
40
#抑制作用#
28
#Treg细胞#
50
#肿瘤患者#
35
#Treg#
46
#头颈部#
29
#颈部#
29