ATS:手术治疗可有效缓解漏斗胸修复术后的获得性胸廓萎缩症
2014-05-20 佚名 dxy
开放修复儿童漏斗胸可导致部分患者胸廓发育不良。幼年期漏斗胸修复术中的肋软骨扩大切除会破坏软骨生长板而抑制骨性胸壁的发育和成熟,导致患者出现获得性胸廓萎缩症(ATD),使患者出现进行性呼吸困难和运动障碍。ATD手术用于提高整体胸廓容积仍存在争议。 美国梅奥诊所的Jaroszewski博士等进行了一项回顾研究,分享了他们手术处理ATD的经验,发现胸骨抬升和前胸壁延长可缓解该类患者的症状。文章最近发表
开放修复儿童漏斗胸可导致部分患者胸廓发育不良。幼年期漏斗胸修复术中的肋软骨扩大切除会破坏软骨生长板而抑制骨性胸壁的发育和成熟,导致患者出现获得性胸廓萎缩症(ATD),使患者出现进行性呼吸困难和运动障碍。ATD手术用于提高整体胸廓容积仍存在争议。
美国梅奥诊所的Jaroszewski博士等进行了一项回顾研究,分享了他们手术处理ATD的经验,发现胸骨抬升和前胸壁延长可缓解该类患者的症状。文章最近发表在Ann Thorac Surg上。
该回顾性研究共纳入了2010年12月至2013年2月间出现ATD的10例男性患者,其中9例接受了手术治疗,并进行了术前和术后对比。
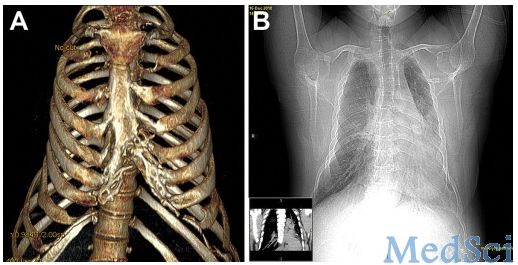
A.一名42岁男性ATD患者的CT三维重建影像。B.该患者的CT和胸片提示胸廓受限和心脏向左侧移位。
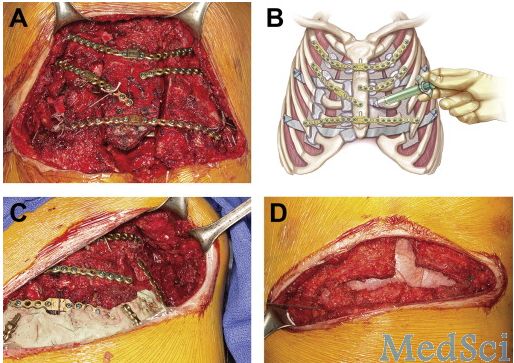
A.在断骨间使用架板来扩大正侧面的胸壁面积,之后使用钛钉固定架板。B.用吊索方式连接缝隙并在缝隙中注入骨胶。C.使用PMMA填充较大的骨缺损,并用钛板固定。D.用不可吸收缝线将胸肌和腹直肌拉至胸部保护中线和下胸壁。
研究结果显示, 8例患者出现轻度并发症,3例患者出现主要并发症,3例患者出现呼吸衰竭并使用呼吸机支持,无再次手术或死亡病例。术后平均随访16个月,所有患者主观上均感受到运动能力提升以及呼吸困难症状减轻。
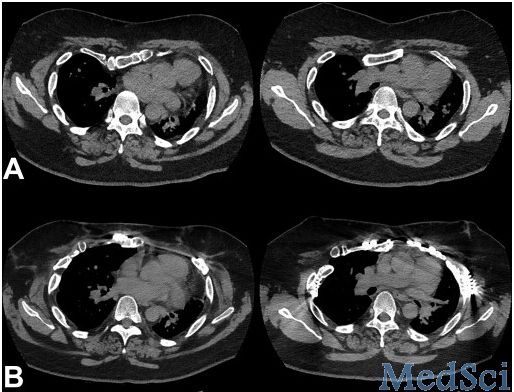
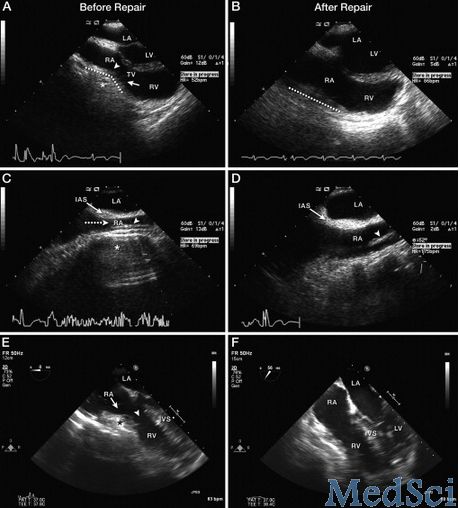
从该研究来看,进行胸骨抬升和前胸壁延长手术可以有效减轻ATD患者的心脏压迫和限制性呼吸困难症状。为手术治疗漏斗胸术后的ATD提供了新的证据。
原始出处:
Jaroszewski DE, Notrica DM, McMahon LE, Hakim FA, Lackey JJ, Gruden JF, Steidley DE, Johnson KN, Mookadam F.Operative management of acquired thoracic dystrophy in adults after open pectus excavatum repair.Ann Thorac Surg. 2014 May;97(5):1764-70.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








不错不错
114
#萎缩#
46
#ATS#
38
#修复术#
39
#手术治疗#
35
#漏斗胸#
49
#获得性#
33