Eur Radiol: PTBD治疗扩张型和非扩张型胆管病变患者预后有何不同?
2021-02-25 shaosai MedSci原创
与胆管扩张的患者相比,非扩张胆管患者行经皮经肝胆道引流术具有更高的并发症发生率和更低的手术成功率。
经皮经肝胆道引流术(PTBD)的主要适应症通常是由肿瘤或炎症后狭窄引起的胆汁淤积。此外,越来越多的非扩张胆管患者行PTBD,主要是为了治疗胆肠吻合部位的术后胆漏。
PTBD最严重的并发症是胰腺炎、出血、胆管与肝动脉或门静脉瘘、假性动脉瘤、胆漏及穿刺造成的气胸或血胸,发生率在8.6–22%之间。与胆管扩张的患者相比,非扩张胆管患者行PTBD具有更高的并发症发生率和更低的手术成功率。
近日,发表在European Radiology杂志的一项研究比较了PTBD在扩张和非扩张胆管患者中的成功率、技术复杂性和并发症发生率。
本项回顾性分析中,我们对我科在5年内进行的所有连续PTBD进行了评价。比较了胆管扩张患者和非扩张胆管患者的技术成功率、技术数据(侧位、透视检查时间、放射线剂量、造影剂用量、 一次性设备的使用)、手术相关的并发症和围手术期死亡率。采用独立的t检验和χ2检验评价统计学意义。
本研究纳入187位患者共行253例手术,253例中有101例为胆管扩张,152例为非胆管扩张。总共有253例手术中有243例手术成功。与非扩张胆管患者相比,PTBD在胆管扩张患者中成功率更高(150/153 vs 93/101;p 0.02)。总体并发症发生率(13%)在胆管扩张和非扩张患者之间没有显著统计学差异。对胆管正常、未扩张的患者进行手术与介入术后出血发生率显著升高相关(5/101 vs. 0/152)。非扩张导管的患者的平均透视时间(42:36±35:39 h vs 30:28±25:10 h;p 0.002)和造影剂用量(66±40 ml vs 52±24 ml; p 0.07) 以及使用一次性用品的比例显著提高。左肝PTBD的透视时间和造影剂用量明显较低。
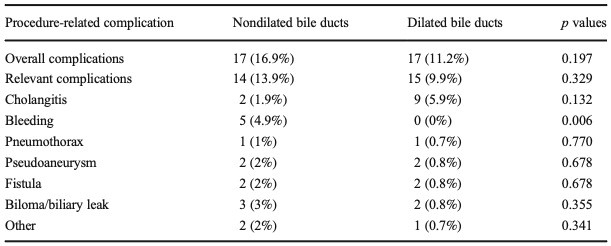
表1 非扩张型和扩张型胆管患者的手术并发症类型和发生率
与胆管扩张的PTBD相比,非扩张胆管的PTBD尽管技术复杂性更高,但总体并发症发生率相似,但出血并发症发生率更高。这提示临床在在介入治疗非扩张胆管患者时,应考虑到这种情况并进行相应的准备和调整以提高患者的手术成功率及预后。
原始出处:
Federico Pedersoli,Anja Schröder,Markus Zimmermann,et al. Percutaneous transhepatic biliary drainage (PTBD) in patients with dilated vs. nondilated bile ducts: technical considerations and complications.DOI:10.1007/s00330-020-07368-6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#患者预后#
33
#扩张#
26
#胆管#
37