Cell Death Differ:非典型NF-κB信号转导通路影响慢性淋巴细胞性白血病的耐药性
2021-01-29 xiaozeng MedSci原创
慢性淋巴细胞性白血病(CLL)是一种原发于造血组织的恶性肿瘤,其主要的问题之一是对治疗产生的后天耐药性。
慢性淋巴细胞性白血病(CLL)是一种原发于造血组织的恶性肿瘤,其主要的问题之一是对治疗产生的后天耐药性。尽管目前已发现和开发了新型的靶向疗法,但疾病的复发仍很常见。
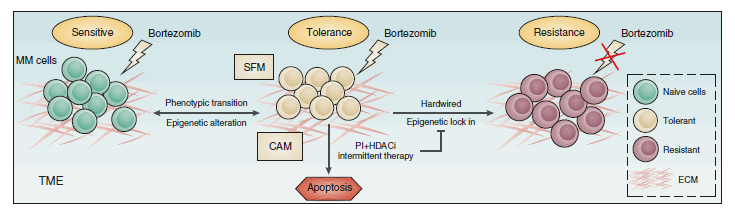
在CLL中,淋巴结(LN)微环境通过诱导抗凋亡Bcl-2成员Bcl-XL、Bfl-1和Mcl-1的表达来传递关键的生存信号,从而导致细胞凋亡作用的阻滞。这也使得CLL对Bcl-2抑制剂Venetoclax(维奈托克,ABT-199)高度敏感。然而,只有极少的患者达到了完全缓解,这可能与微环境诱导的抗性产生相关。
由于在LN微环境中CLL Bcl-XL的实际调控情况目前尚不清楚,因此,需要深入了解诱导Bcl-XL表达的相关信号,以评估CLL和其他病理学中靶向治疗的替代选择。研究人员在各种候选LN信号中评估驱动Bcl-XL表达的信号。
Bcl-XL在CLL的venetoclax耐药中起着重要作用
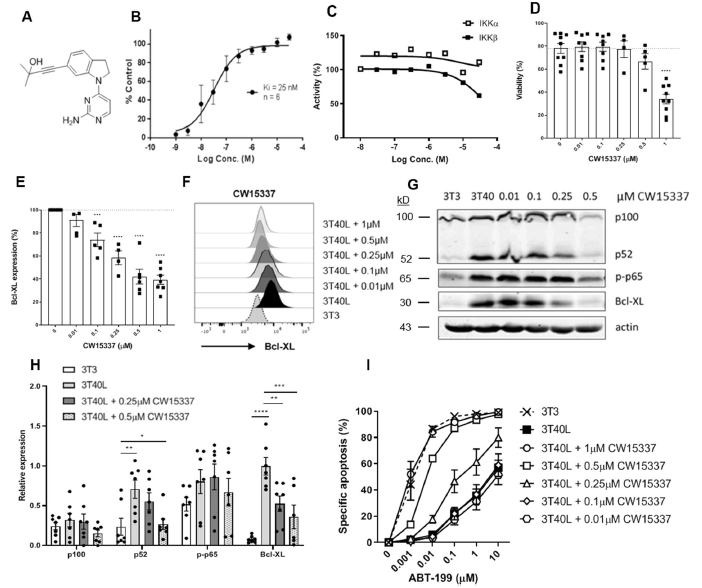
研究人员发现,CD40诱导的NF-κB信号转导通路占主导地位,这也导致经典和非经典NF-κB信号通路均被激活。研究人员证实,Bcl-XL的表达首先被经典的NF-κB途径所诱导,随后通过NIK的稳定化并由非经典的NF-κB信号增强和维持。NF-κB亚基p65和p52均可与Bcl-XL的启动子区域结合,并在CD40刺激后激活转录。
此外,进一步的研究显示,经典的NF-κB信号转导通路与Bfl-1的表达水平相关,而相反的,Mcl-1则不受NF-κB的转录调控。最后,研究人员通过靶向NIK的新型化合物来选择性的抑制非经典的NF-κB信号通路,发现Venetoclax耐药性CLL细胞又重新对Venetoclax致敏。
靶向非典型NF-κB信号通路下调Bcl-XL的表达并增加venetoclax敏感性
总而言之,该研究结果显示,通过靶向干扰非经典的NF-κB信号转导通路,CLL会趋向对细胞凋亡作用敏感。
原始出处:
Haselager, M., Thijssen, R., West, C. et al. Regulation of Bcl-XL by non-canonical NF-κB in the context of CD40-induced drug resistance in CLL. Cell Death Differ (25 January 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
0
#Differ#
38
#细胞性#
32
#Cell#
31
#淋巴细胞#
30
#慢性淋巴细胞性白血病#
27
#非典型#
44
#Death#
33