EHJ:“宝藏药”沙库巴曲-缬沙坦作为治疗HFpEF合并难治性高血压患者的疗效
2021-08-21 MedSci原创 MedSci原创
高血压和射血分数保留的心力衰竭(HFpEF)之间密切相关。
众所周知,高血压和射血分数保留的心力衰竭(HFpEF)之间密切相关。左心室肥大、动脉硬化和肾功能损害可能有助于这种综合征的发展。此外,许多HFpEF患者仍有高血压,治疗这种合并症是对这种心力衰竭表型的人推荐的少数治疗方法之一。
难治性高血压的正式定义是:尽管使用了三种不同类别的降压药,包括血管紧张素转换酶(ACE)抑制剂或血管紧张素受体阻断剂(ARB)、钙通道阻断剂和利尿剂,但血压仍持续高于目标值。事实上,"难治性高血压 "在HFpEF患者中十分常见,有10-20%的患者受到影响。
抑制肾小球蛋白酶提供了另一种降低血压的方法。 治疗8周后,与缬沙坦相比,使用沙库巴曲-缬沙坦的收缩压降低了6.01(95%CI:-9.01~-3.02mmHg)。因此,沙库巴曲缬沙坦随后被开发为一种治疗心力衰竭的药物,采用每天两次的给药方案。
在一项针对266名患者的2期随机试验中,沙库巴曲缬沙坦 97/103mg,每天两次,与缬沙坦160mg,每天两次进行了比较。这项试验表明,经过12周的治疗,沙库巴曲缬沙坦与缬沙坦相比,收缩压降低了6.4mmHg。
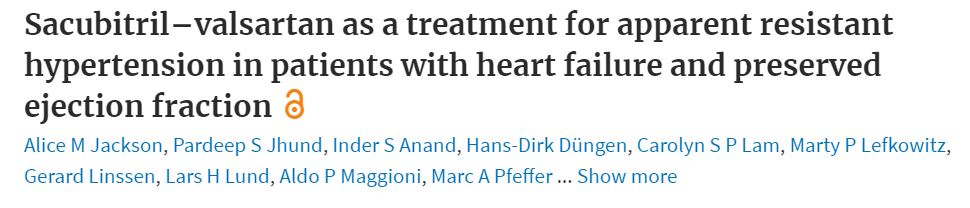
近期,英国格拉斯哥大学的心血管专家开展了一项名为“PARAGON-HF试验”,旨在研究与缬沙坦相比,沙库巴曲缬沙坦对HFpEF患者 "难治性高血压"的影响,结果发表在《欧洲心脏病杂志》EHJ上。
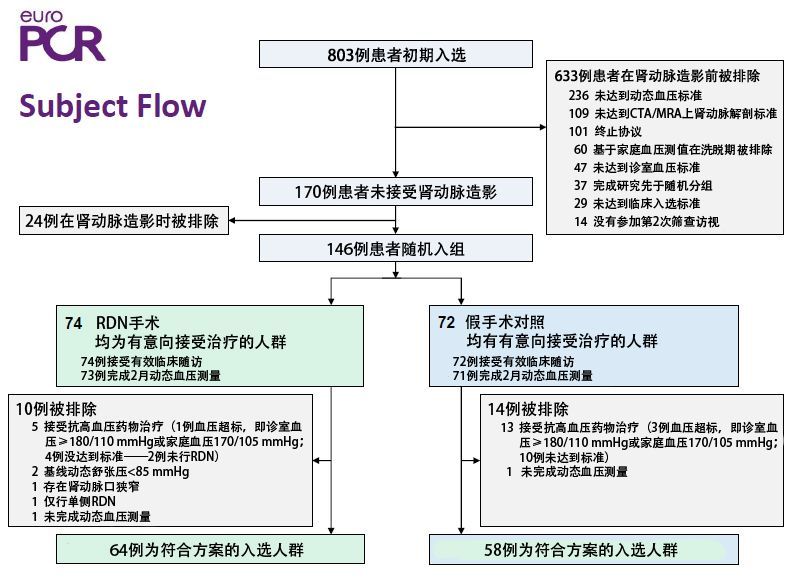
在这项事后分析中,根据缬沙坦试验结束时的收缩压对患者进行分类(n = 4795)。难治性高血压被定义为尽管使用了缬沙坦、钙通道阻滞剂和利尿剂治疗,收缩压仍≥140 mmHg(如果是糖尿病,则≥135 mmHg)。明显的矿物皮质激素受体拮抗剂(MRA)耐受性高血压被定义为尽管接受了上述治疗和MRA,收缩压仍≥140 mmHg(如果是糖尿病,则≥135 mmHg)。主要结果是心力衰竭住院总数和心血管原因死亡的综合。
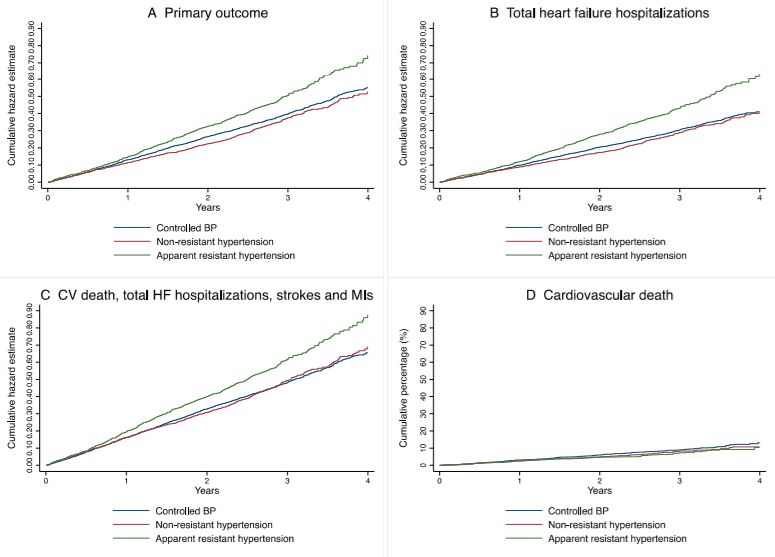
总的来说,731名患者(15.2%)有明显的难治性高血压,135名(2.8%)有明显的MRA耐受性高血压。与收缩压得到控制的患者相比(13.4/100人年),难治性高血压患者的心血管率高28%(17.3/100人年,HR=1.28)。
根据高血压类别的危险和生存曲线。(A) 主要结果。(B) 心衰住院总数。(C)心血管死亡、心衰住院总数、中风和心肌梗死。(D) 心血管疾病死亡
与缬沙坦相比,沙库巴曲-缬沙坦在第4周和第16周,难治性高血压 [-4.8(-7.0至-2.5)和3.9(-6.6至-1.3)mmHg]和明显MRA抵抗性高血压[-8.8(-14.0至-3.5)和-6.3(-12.5至-0.1)mmHg]的收缩压下降幅度更大。
到第16周,明显抵抗性高血压患者的收缩压得到控制的比例在沙库巴曲-缬沙坦组为47.9%,而在缬沙坦组为34.3%,几率增加78%(OR=1.78,95%CI 1.30-2.43)。在有明显MRA抗性的高血压患者中,其比例分别为43.6%和28.4%(OR=2.63,95%CI 1.18-5.89)。
综上,对于HFpEF合并难治性高血压的患者,“宝藏药物”沙库巴曲缬沙坦表现优异。
参考文献:
Sacubitril–valsartan as a treatment for apparent resistant hypertension in patients with heart failure and preserved ejection fraction, European Heart Journal, 2021;, ehab499, https://doi.org/10.1093/eurheartj/ehab499
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















#PE#
31
#HFpEF#
49
#缬沙坦#
43
#高血压患者#
38
#难治性#
31
谢谢梅斯提供这么好的信息,学到很多
0