Stroke:支架可作为前循环大脑大动脉闭塞取拴术失败后补救治疗
2016-07-31 MedSci MedSci原创
我们假设永久性支架可作为前循环大动脉闭塞支架取栓失败后的补救治疗。比较了患者取栓失败后使用永久性支架和未使用的结局。 研究方法:回顾性评估韩国2010年9月至2015年9月间2
我们假设永久性支架可作为前循环大动脉闭塞支架取栓失败后的补救治疗。比较了患者取栓失败后使用永久性支架和未使用的结局。
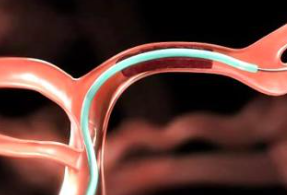
研究方法:回顾性评估韩国2010年9月至2015年9月间208例进行前循环大动脉闭塞后支架取栓病例。改良溶栓单独伴随支架取栓或者同时使用Penumbra装置在155位患者(74.5%)获得脑缺血 2b-3再通。此外8位患者(3.8%)通过注射尿激酶或者糖蛋白IIb/IIIa抑制剂获得改良溶栓。剩余45人(21.6%), 17人放置了支架(支架组:平均年龄,68岁),28例未放置支架(非支架组:平均年龄,72岁)。支架组脑缺血 2b-3再通改良溶栓比率进行评估,组间的临床结局进行对比。
结果:组间临床表现,实验室发现,初始NIHSS评分,前循环大血管闭塞定位,开始到穿刺时间都无差异。支架组14例患者(83.3%)获得了改良溶栓脑缺血 2b-3再通。与非支架组(MRS评分0-2, 7.1%;脑疝形成,42.9%)相比支架组预后较好(MRS评分0-2, 35.3%),有更少的脑疝形成 (11.8%),( P<0.05 for both) 。症状性脑出血及死亡率在支架组 (症状性脑出血, 11.8%; 死亡率, 23.5%)和非支架组(症状性脑出血, 14.3%; 死亡率, 39.3%)无差异。
结论:永久性支架可能是前循环大动脉闭塞取栓失败的补救方法。因为此研究样本量较小,仍需要大型前瞻性研究进一步确认。
原始出处:
Baek JH1, Kim BM2, Kim DJ1, et al,Stenting as a Rescue Treatment After Failure of Mechanical Thrombectomy for Anterior Circulation Large Artery Occlusion,Stroke. 2016 Jul 21. pii: STROKEAHA.116.014073. [Epub ahead of print]
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#动脉闭塞#
49
#大动脉闭塞#
47
文章很好,继续关注
105
学习了,文章有深度,值得探究。
94
很好,不错,以后会多学习
98