动脉粥样硬化是心血管系统最常见的一种疾病,通常以中、老年居多。但是,近年来,也多见于青壮年人群。大量的研究表明,IL-6是动脉粥样硬化血栓形成的关键因素。然而,在动脉粥样硬化高风险但没有系统性炎症疾病的个体中,抑制IL-6的安全性和有效性尚不明确。
Ziltivekimab(泽韦奇单抗),是一种针对IL-6配体的人单克隆抗体。与其他临床可用的IL-6抑制剂不同,泽韦奇单抗是专门为动脉粥样硬化治疗而研发的。针对IL-6配体而不是IL-6受体,泽韦奇单抗可以较低剂量使用,对脂质水平、血液学指标和肝功能的不良影响较小。
近日,来自美国哈佛医学院布莱根妇女医院心血管疾病预防中心的Paul M Ridker课题组研究人员在《The Lancet》上发表了题为“IL-6 inhibition with ziltivekimab in patients at high atherosclerotic risk (RESCUE): a double-blind, randomised, placebo-controlled, phase 2 trial”的研究成果,提出泽韦奇单抗可明显减少与动脉粥样硬化有关的炎症和血栓形成。
为了探讨泽韦奇单抗是否能安全有效地减少高心血管风险患者的炎症和血栓形成,研究人员在美国40个临床点进行了一项随机、双盲、2期临床试验。
入选标准为18岁或以上,中度至重度慢性肾脏疾病以及至少2 mg / L的高敏感性CRP。参与者被随机分配(1:1:1:1)进行皮下给药,皮下注射7.5 mg/15 mg或30 mg的安慰剂或泽韦奇单抗, 每4周一次直至24周。在2019年6月17日至2020年1月14日之间,共招募了264名受试者,其中66名受试者被随机分配到四个治疗组中。
主要结果是与安慰剂相比,用每4周一次直至24周治疗12周后高敏CRP相对于基线的百分比变化,以及在治疗24周内收集的其他生物标志物和安全性数据。在意向性治疗人群中进行了初步分析。在接受至少一剂指定治疗的所有患者中评估安全性。
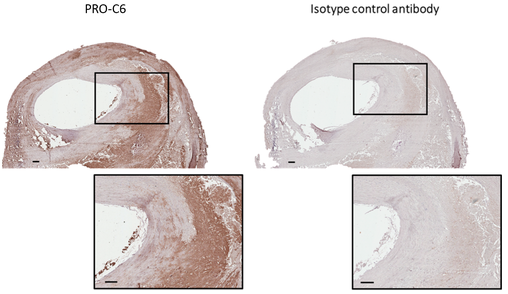
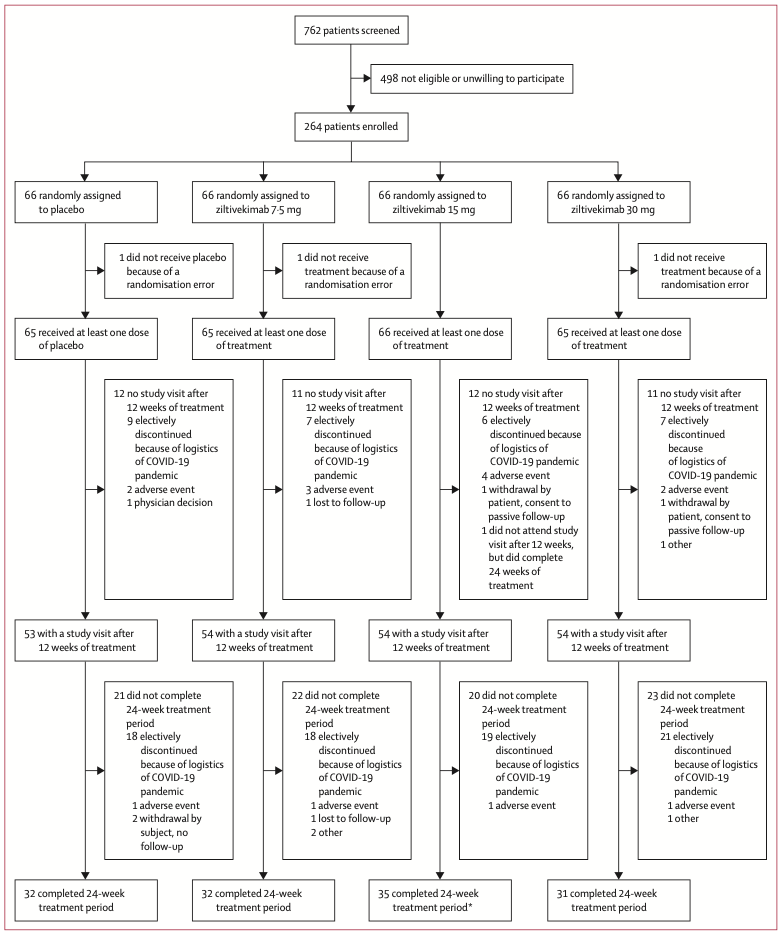 试验设计
试验设计
各治疗组的基线临床特征相似。治疗12周后,所有泽韦奇单抗治疗组的高敏CRP水平降低幅度均明显大于安慰剂组。因此,在调整分层后,安慰剂组和韦奇单抗组之间高敏CRP的百分比变化中位数差异显着。也就是说,治疗12周后,与安慰剂组相比,泽韦奇单抗治疗可将高敏CRP降低至少50%,并且最终高敏CRP低于2 mg / L。
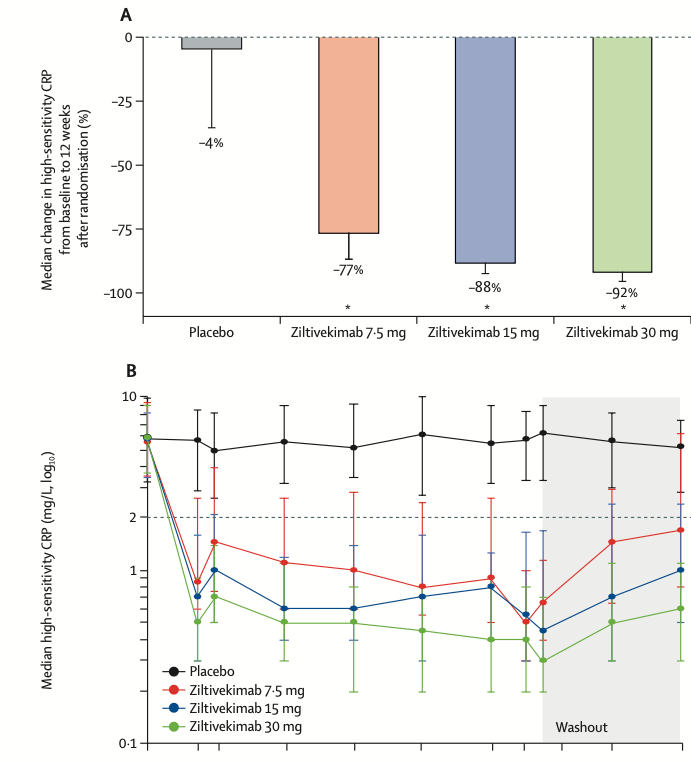
各治疗组高敏CRP变化
各治疗组的每个受试者在12周时的高敏CRP百分比变化的瀑布图显示,安慰剂组的变化分布广泛,但是大多数接受泽韦奇单抗治疗的受试者的高敏CRP降低幅度很大且持续降低。
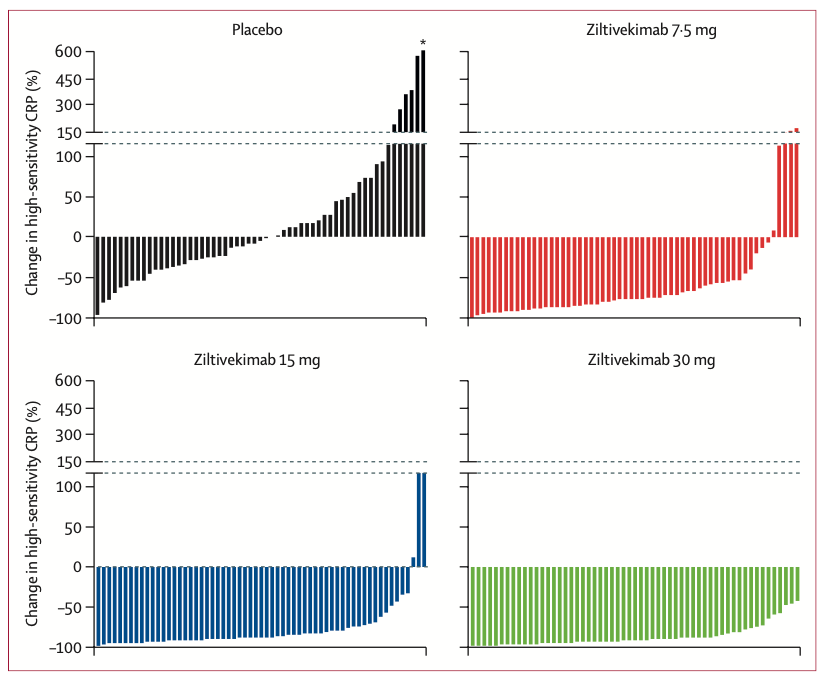
各治疗组中高敏CRP百分比变化
并且,研究人员发现泽韦奇单抗可显着减低脂蛋白的水平,并少量增加APOB、HDL胆固醇和APOA1。与安慰剂组相比,泽韦奇单抗组的甘油三酯增加。还观察到了血纤蛋白原,血清淀粉样蛋白A,触觉珠蛋白,分泌性磷脂酶A2和脂蛋白的剂量依赖性降低。此外,安慰剂组和泽韦奇单抗治疗组之间eGFR、尿白蛋白与肌酐的比例未见差异。
在整个试验过程中,未观察到严重的注射相关反应。安慰剂组有1例心血管死亡,泽韦奇单抗 7.5 mg组有1例非致命性心肌梗塞,泽韦奇单抗15 mg组有1例非致命性心肌梗塞。

不良反应
简而言之,研究表明泽韦奇单抗可显着减少与动脉粥样硬化有关的炎症和血栓形成。研究人员表示,在此数据的基础上,他们将进行一项大规模的心血管试验,研究泽韦奇单抗在慢性肾脏疾病、高敏CRP升高和已确定的心血管疾病患者中的作用。让我们共同期待该药可以造福广大动脉粥样硬化患者。
原始出处:
Paul M Ridker, et al. IL-6 inhibition with ziltivekimab in patients at high atherosclerotic risk (RESCUE): a double-blind, randomised, placebo-controlled, phase 2 trial. The Lancet, 2021. DOI:https://doi.org/10.1016/S0140-6736(21)00520-1.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#粥样硬化#
44
#Lancet#
36
#高危患者#
34
#IL-6#
51
不懂
57
顶刊就是不一样,质量很高,内容精彩!学到很多
44