J Allergy Clin Immunol:哮喘和过敏性鼻炎患者中对TLR7/8激动剂的鼻粘膜干扰素和CCL13反应增加
2020-08-16 AlexYang MedSci原创
急性呼吸道病毒感染是呼吸道发病和死亡的主要原因,尤其是对于已有肺部疾病如哮喘的患者。Toll样受体(TLRs)在早期病毒检测和激活呼吸道黏膜先天性免疫中起着关键作用,但目前还没有可靠、方便的方法来检测
急性呼吸道病毒感染是呼吸道发病和死亡的主要原因,尤其是对于已有肺部疾病如哮喘的患者。Toll样受体(TLRs)在早期病毒检测和激活呼吸道黏膜先天性免疫中起着关键作用,但目前还没有可靠、方便的方法来检测呼吸道黏膜的先天性免疫反应。最近,有研究人员评估了健康和过敏志愿者中对先天免疫刺激的免疫响应情况,并进行了比较。
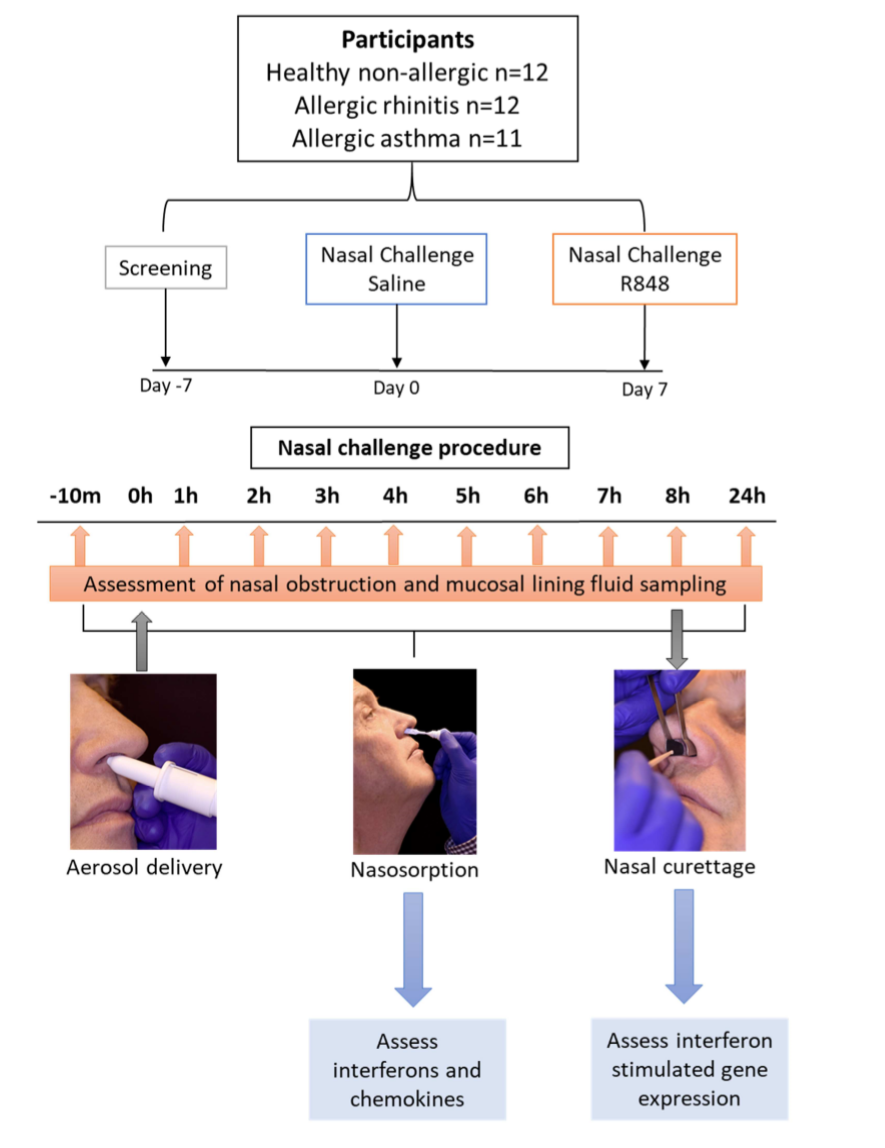
R848鼻挑战流程图
研究包括了健康非过敏参与者(n=12),过敏性鼻炎参与者(n=12)和哮喘过敏性鼻炎参与者(n=11),并分别进行TLR7/8激动剂瑞喹莫德(R848)或者生理盐水喷雾处理。研究发现,R848具有良好的耐受性并显著诱导鼻粘膜液体中的干扰素(IFN)-α2a、IFN-γ、促炎细胞因子(TNF-α、IL-2和IL-12p70)和化学因子(CXCL10、CCL2、CCL3、CCL4和CCL13),并不引起全身免疫激活。过敏性鼻炎参与者或者具有哮喘的过敏性鼻炎参与者与健康对照相比IFN-α2a增加,CCL3和CCL13响应增加;而那些具有哮喘的参与者的干扰素刺激基因DDX58、MX1和IFIT3诱导增加。
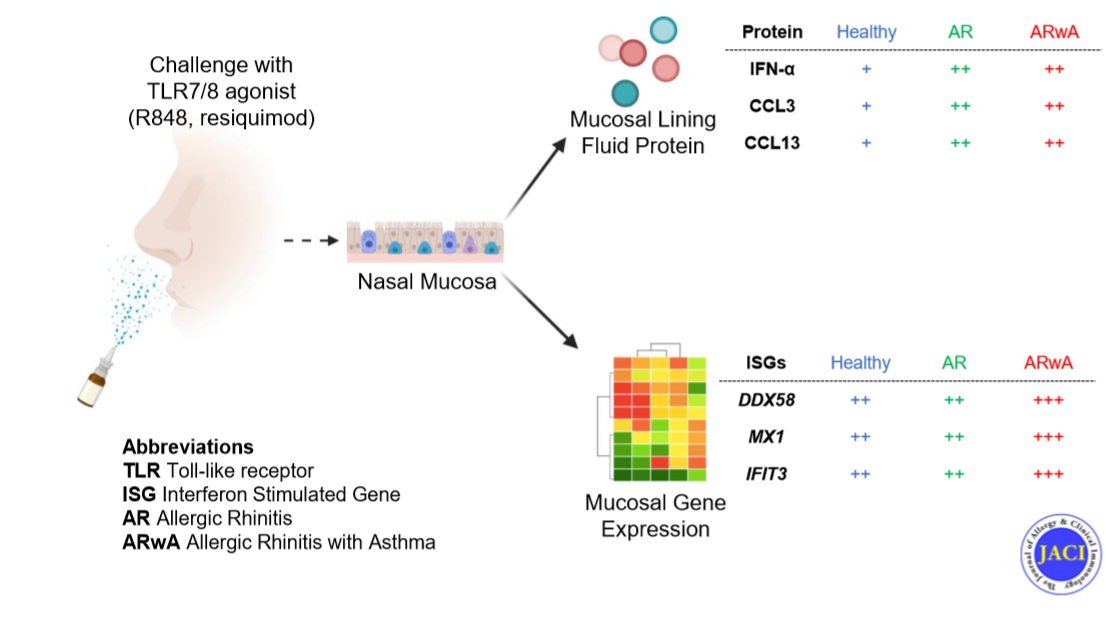
TLR7和8激动剂的鼻粘膜干扰素和CCL13反应增加
最后,研究人员指出,对R848的响应可以对鼻粘膜先天免疫响应进行简单的评估,具有过敏障碍的患者鼻粘膜干扰素和化学因子响应增加。他们的研究结果强调了过敏个体中鼻粘膜先天免疫响应的异常调控在病毒暴露结果中具有的作用。
原始出处:
Akhilesh Jha, Ryan S Thwaites, Tanushree Tunstall et al. Increased nasal mucosal interferon and CCL13 response to a TLR7/8 agonist in asthma and allergic rhinitis. J Allergy Clin Immunol. Jul 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#TLR#
35
#过敏性#
31
#鼻粘膜#
35
#TLR7#
41
#粘膜#
39
#ALL#
33
#激动剂#
26
学习了!
94