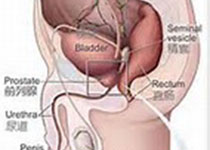
Prostate Cancer P D:经历前列腺活检男性的直肠穹窿氟喹诺酮抗性细菌预测因子研究
2018-10-15 AlexYang MedSci原创
氟喹诺酮(FQ)抗性直肠穹窿菌群与经历经直肠超声引导的前列腺穿刺活检(TRUS-PNB)的男性的感染性并发症相关。最近,有研究人员确定了能够预测FQ抗性直肠培养物的患者因素,这些患者经历了直肠超声引导的前列腺穿刺活检。研究发现,在分析的6179个直肠拭子中,4842(78%)名为FQ敏感性,1337名(22%)为FQ抗性。在单变量分析中,年龄的增加、优先TRUS-PNB、获得的更高的活检核心数目、
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#喹诺酮#
49
#前列腺活检#
30
#Prostate Ca#
34
#抗性#
32
学习了谢谢分享
69
#活检#
26
#预测因子#
20
#ROS#
27
#氟喹诺酮#
28
#PRO#
26