Nature:抗癌新疗法——PLK4抑制剂
2020-09-19 医药魔方 医药魔方
9月9日,最新发表在Nature杂志上的一篇论文中,来自约翰霍普金斯大学和牛津大学的科学家们报道了阻止一种人类乳腺癌细胞增殖的潜在方法。
9月9日,最新发表在Nature杂志上的一篇论文中,来自约翰霍普金斯大学和牛津大学的科学家们报道了阻止一种人类乳腺癌细胞增殖的潜在方法[1]。这种新方法靶向癌细胞分裂所依赖的一种基于中心粒的关键机制。研究揭示,使用PLK4抑制剂centrinone处理过表达TRIM37蛋白的乳腺癌细胞会破坏中心粒(centriole)的活性,抑制癌细胞生长。
由于这类癌细胞的分裂依赖于中心粒,但正常细胞不存在这种情况,因此,研究者们认为,抑制PLK4(polo-like kinase 4)或其它中心粒功能调节因子有望成为选择性靶向这种乳腺癌亚型的一种新策略。
来源:Nature
具体来说,在该研究中,科学家们重点研究了17q23染色体区域拷贝数增加的乳腺癌细胞,这类细胞的分裂高度依赖中心粒(中心粒可组织微管蛋白,形成微管结构,也可在细胞分裂期间帮助分离DNA)。
在位于17q23区域的大约40个蛋白质编码基因中,研究人员注意到TRIM37的存在,该基因先前已被证明与中心粒功能有关。由于蛋白质PLK4调节中心粒的产生,研究人员推测,阻断它可能会破坏那些TRIM37过表达的乳腺癌细胞的分裂过程。
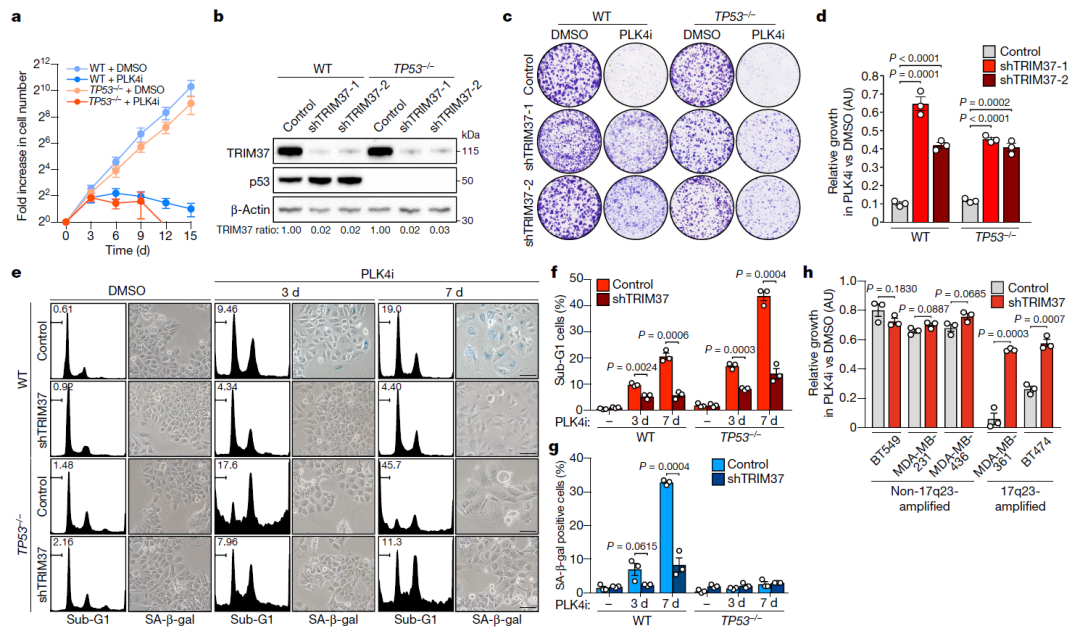
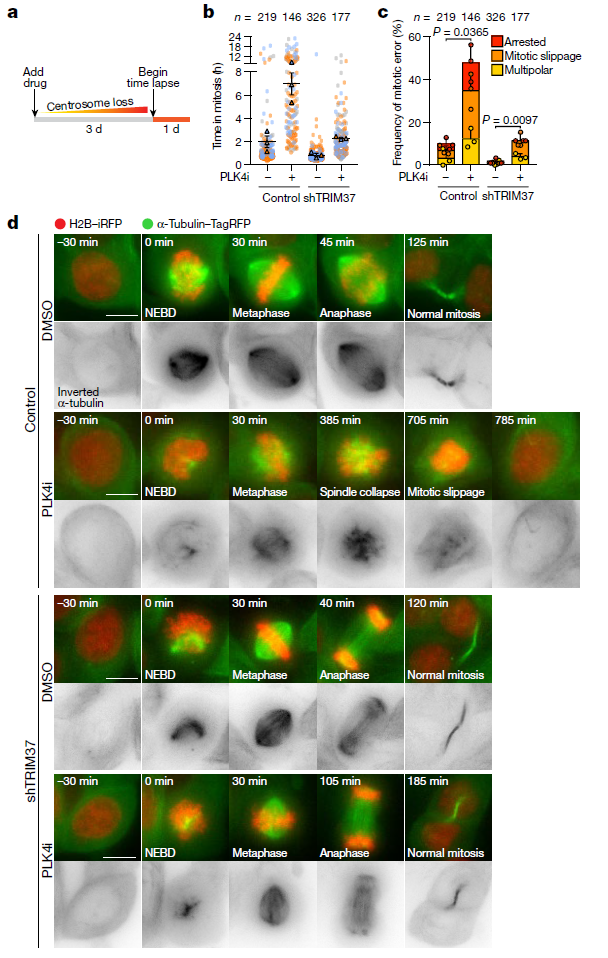
PLK4抑制剂与TRIM37扩增可导致合成致死(来源:Nature)
他们将PLK4抑制剂centrinone加入到TRIM37水平正常的乳腺癌细胞中,发现即使中心粒被药物阻断了,细胞仍能正常分裂。但是,如果用这种药物处理TRIM37水平较高的乳腺癌细胞,这些细胞就会停止生长或死亡。
在TRIM37扩增癌细胞中,PLK4抑制剂触发了有丝分裂障碍(来源:Nature)
先前的研究表明,正常细胞在没有中心粒的情况下也能分裂,这是因为中心粒外周物质(pericentriolar material)会接管这项任务。而在这项研究中,科学家们发现,TRIM37过表达可导致中心粒外周物质的降解。这就有效消除了在没有中心粒的情况下癌细胞分裂所能使用的替代途径。
来源:Nature
研究人员认为,这一发现为使用中心体靶向药物治疗17q23扩增型乳腺癌提供了理论依据。
「我们的想法是鉴定出TRIM37水平高的肿瘤,再使用PLK4抑制剂选择性地杀死癌细胞,使健康细胞相对不受伤害。」论文共同通讯作者Andrew Holland博士说。
除了Holland博士及其合作伙伴的这项新发现,同日发表在Nature杂志上的另一篇题为「TRIM37 controls cancer-specific vulnerability to PLK4 inhibition」的论文也揭示,TRIM37控制着癌症响应PLK4抑制剂特异性的脆弱性[2]。
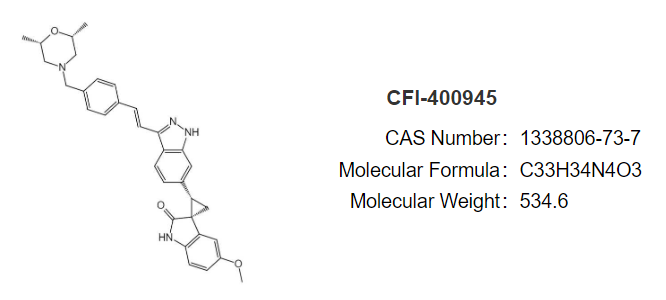
CFI-400945的结构(来源:NaxtPharma)
事实上,早前已有研究揭示,PLK4在多种实体肿瘤中过表达,且这种高表达与不良的临床结果相关,而通过RNA干扰阻断癌细胞中的PLK4表达导致了有丝分裂缺陷和细胞死亡,因此PLK4被鉴定为一个潜在的抗癌靶点。
目前已有一款PLK4抑制剂进入临床开发阶段。这款名为CFI-400945的候选药物由总部位于纽约的Treadwell Therapeutics开发,是一款first-in-class的口服小分子,目前正在联合阿斯利康的PD-L1抑制剂度伐利尤单抗(Imfinzi)在难治性三阴性乳腺癌患者中开展一项II期试验(NCT04176848)。此外,CFI-400945针对复发或难治性急性髓系白血病或骨髓增生异常综合症和前列腺癌等适应证的临床试验也在进行中。不过,值得一提的是,此前,在没有任何生物标志物预先筛选患者的情况下,该药物在针对实体肿瘤患者的I期试验中诱导了有限的反应。
Holland博士称,他们正在寻找更稳定的PLK4抑制剂以供进一步研究,并在试图发现对PLK4抑制敏感的其他人类癌症类型。
原始出处:
Zhong Y. Yeow et al. Targeting TRIM37-driven centrosome dysfunction in 17q23-amplified breast cancer. Nature(2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#抗癌新疗法#
42
#Nat#
23
#抑制剂#
19
#新疗法#
33