CELL METAB:清除衰老细胞不仅不能抗衰老,还有害健康?
2020-06-20 MedSci原创 MedSci原创
衰老细胞的积累可导致许多与年龄相关的表型和病理。因此,有人提出,去除衰老细胞可能会延长寿命。
衰老细胞的积累可导致许多与年龄相关的表型和病理。因此,有人提出,去除衰老细胞可能会延长寿命。
最近,研究人员生成了两个针对衰老的最佳特征标志物p16Ink4a的基因敲入小鼠模型。
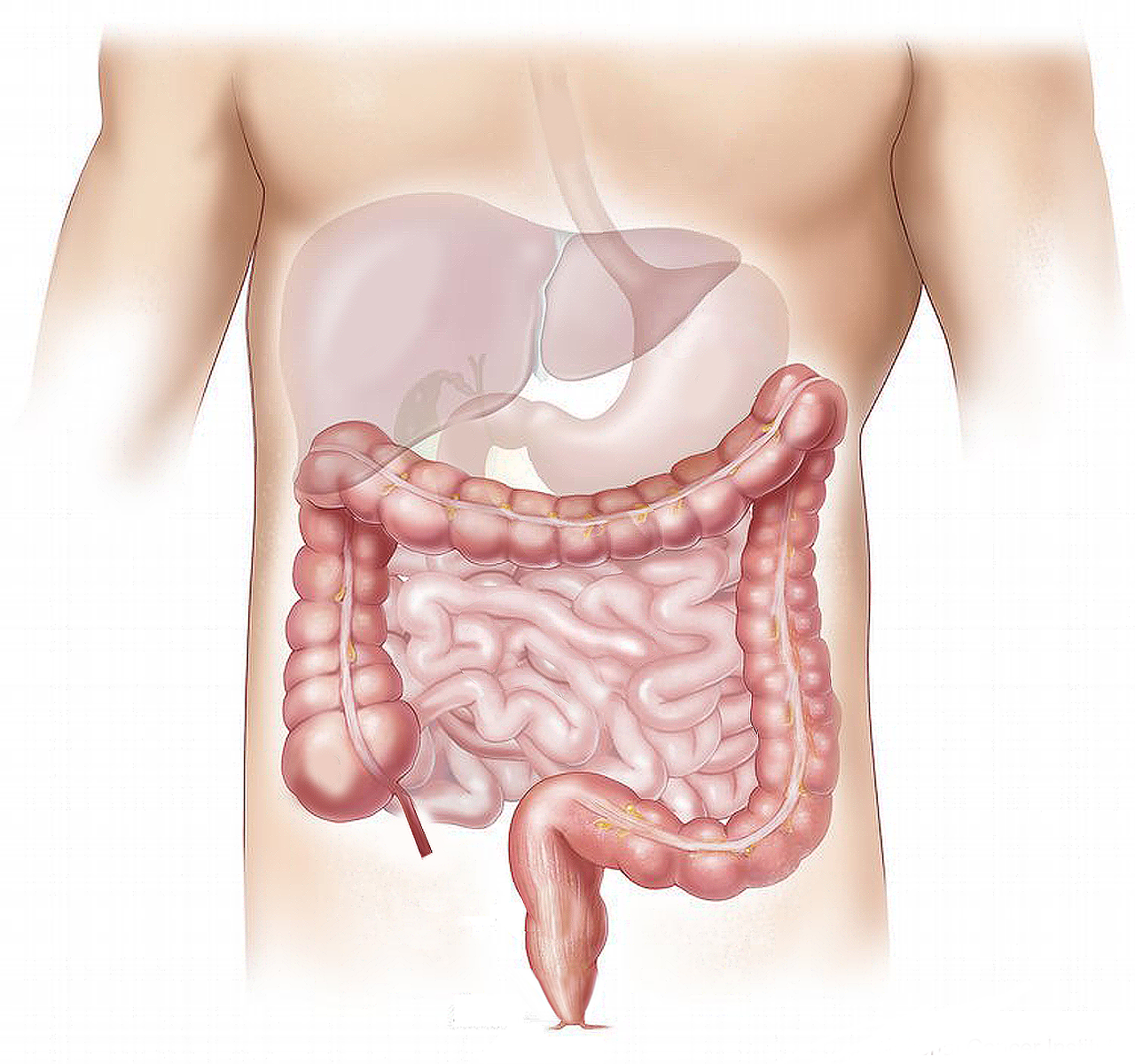
使用遗传谱系追踪方法,研究人员发现,年龄诱导的p16高表达的衰老是一个缓慢的过程,在10-12个月龄左右表现出来。大多数p16高表达细胞是血管内皮细胞,主要在肝窦细胞(LSECs)中,较少的是巨噬细胞和脂肪细胞。
反过来,持续或急性消除p16高表达衰老细胞会破坏了血液-组织屏障,导致随后的肝脏和血管周围组织纤维化和健康恶化。
该研究数据还表明,衰老的LSECs在清除后不会被替换,在衰老的机体中具有重要的结构和功能作用。
反过来,延缓衰老或替换衰老的LSECs可以代表一个强大的延缓衰老的策略。
原始出处:
Laurent Grosse et al. Defined p16High Senescent Cell Types Are Indispensable for Mouse Healthspan, Cell Metabolism (2020). DOI:https://doi.org/10.1016/j.cmet.2020.05.002
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Meta#
32
#MET#
26
#Cell#
20
#CEL#
24