JACC:常规超声或X线的使用以及经股动脉TAVR后出血的风险
2020-06-17 xiangting MedSci原创
FCA或2D-US引导股动脉穿刺可能出现血管和出血并发症。
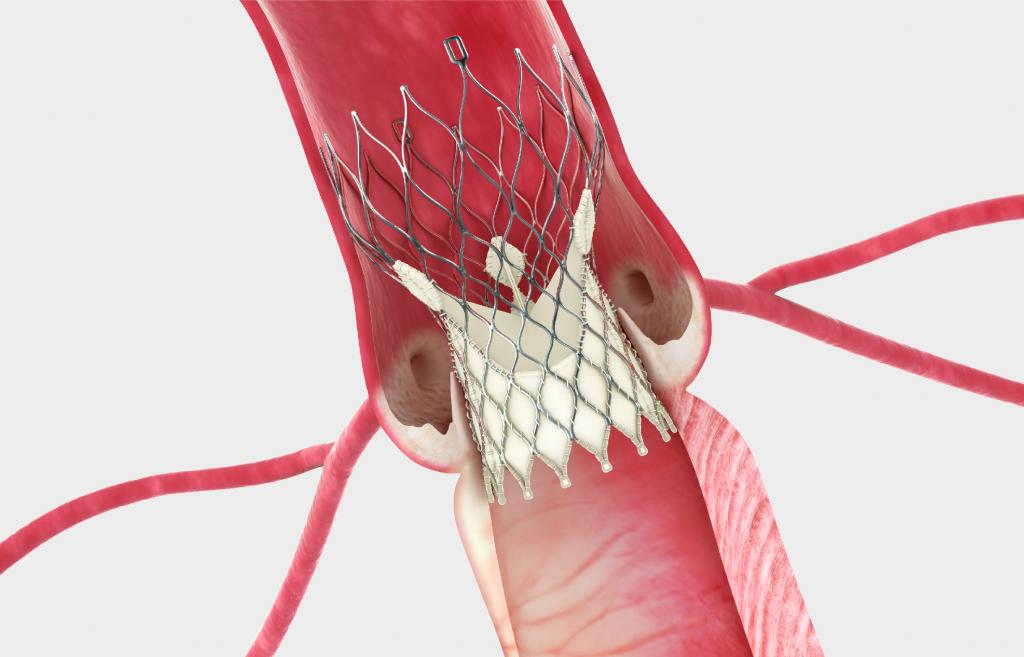
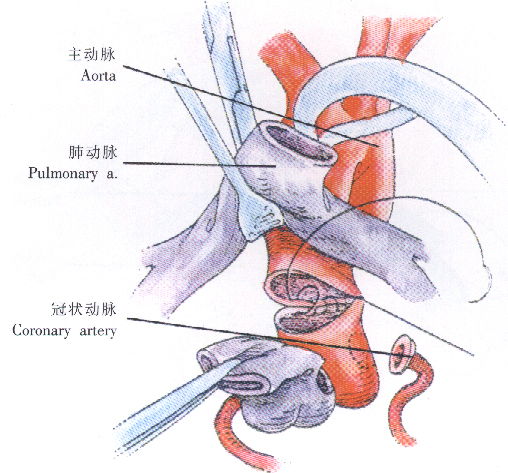
这项研究旨在探讨经股动脉经导管主动脉瓣置换术(TAVR)患者常规使用二维超声的益处。
二维超声(2D-US)可以减少经股动脉入路经皮冠脉介入治疗患者的通路相关血管并发症(VCs)和出血。2D-US对经股动脉TAVR患者是否有潜在相似的益处尚未得到系统研究。
使用来自英国两个相邻大手术量TAVR中心的5年回顾性观察数据,这两个中心TAVR股动脉穿刺时使用2种不同的技术(中心1:X线透视和对侧血管造影[FCA],中心2:2D-US),比较了通路相关VCs或出血的发生率。
总的来说,该研究纳入1,171名患者(FCA,n=624;2D-US,n=529)。两组的基线临床和手术特征相似。不同股动脉穿刺技术VCs、出血或其复合的风险没有差异(分别为FCA vs.2D-US:6.7%[95%置信区间(CI):4.9%-8.9%] vs.6.8%[ 95%CI:4.8%-9.3%];p=0.63;6.1%[95%CI:4.4%-8.2%] vs. 6.4%[95%CI:4.8%-9.3%];p=0.70和9.8%[95%CI:7.6%-12.4%] vs.9.8%[95%CI:7.4%-12.7%];p=0.76),并当分析仅限于主要VCs或威胁生命和大出血的复合时,也没有差异。
FCA或2D-US引导穿刺可能发现血管和出血并发症。需要进一步的研究来确定和评估减少该患者人群围手术期VCs和出血的替代策略。
原始出处:
Guy Witberg. Routine Ultrasound or Fluoroscopy Use and Risk of Vascular/Bleeding Complications After Transfemoral TAVR. JACC:Cardiovascular Interventions. 22 June 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#股动脉#
40
#JACC#
23
#AVR#
37
#经股动脉#
48
#X线#
32
#ACC#
35