Arthritis Rheumatol:无论是否伴有发热,卡那单抗都能快速持续地改善系统性幼年特发性关节炎
2021-05-16 MedSci原创 MedSci原创
全身性幼年特发性关节炎(JIA)表现为关节炎和全身性特征,如发热、皮疹、肝脾肿大和淋巴结病。卡那单抗是一种选择性的抗IL-1β单克隆抗体,已证明在系统性JIA中起效快,随后在相当多的患者中出
全身性幼年特发性关节炎(JIA)表现为关节炎和全身性特征,如发热、皮疹、肝脾肿大和淋巴结病。卡那单抗是一种选择性的抗IL-1β单克隆抗体,已证明在系统性JIA中起效快,随后在相当多的患者中出现了与停用糖皮质激素有关的持续疗效,并具有良好的长期安全性。然而,在开始治疗时,有发热或其他系统性特征(皮疹、淋巴腺病或肝脾肿大)的系统性JIA患者与没有发热或其他系统性特征的患者之间对卡那单抗反应的潜差异知之甚少。近日,研究人员评估了卡那单抗的长期疗效和安全性,并探讨了对开始治疗时有或没有发热的系统性幼年特发性关节炎(JIA)患者的反应预测,研究结果已发表于Arthritis Rheumatol。

入院时,活动性系统性JIA患者(2至<20岁)开始使用卡那单抗(4mg/kg,每4周皮下注射)。疗效指标包括改编的美国风湿病学会(ACR)儿科50/70/90标准、青少年关节炎疾病活动度评分(JADAS),以及临床非活动性疾病和药物治疗的临床缓解,由JADAS或ACR标准评估。
结果,123名患者中(70名有发热,52名无发热[1名患者未报告发热情况]),84名(68.3%)完成了研究(中位持续时间1.8年)。到第15天,两个亚组的疗效(适应ACR小儿科50/70/90/100)具有可比性(发烧者60.0%/48.6%/37.1%/24.3%,不发烧者67.3%/48.1%/34.6%/19.2%),此后进一步提高。到第6个月,根据JADAS或ACR标准,发热患者中分别有17人(24.3%)和26人(37.1%)达到临床缓解,无发热患者中分别有9人(17.3%)和12人(23.1%)达到临床缓解。根据JADAS或ACR标准,发烧患者的临床缓解发生的中位时间分别为57天和30天,无发烧患者的中位时间分别为58天和142天。根据JADAS(OR,13;95%CI:4,42;P<0.0001)或糖皮质激素停用(OR,19;95%CI :3,114;P=0.002),第15天之前适应ACR小儿50的反应是实现临床缓解的最强预测因素。在进入研究时71名(57.7%)接受糖皮质激素的患者中,27名(38.0%)停止使用糖皮质激素,21名(29.6%)剂量达到<0.2mg/kg/day,发烧和不发烧的患者之间没有差异;13名患者(10.6%)耐受了持续的卡那单抗剂量减少到每4周2mg/kg。没有新的不良事件的发生。
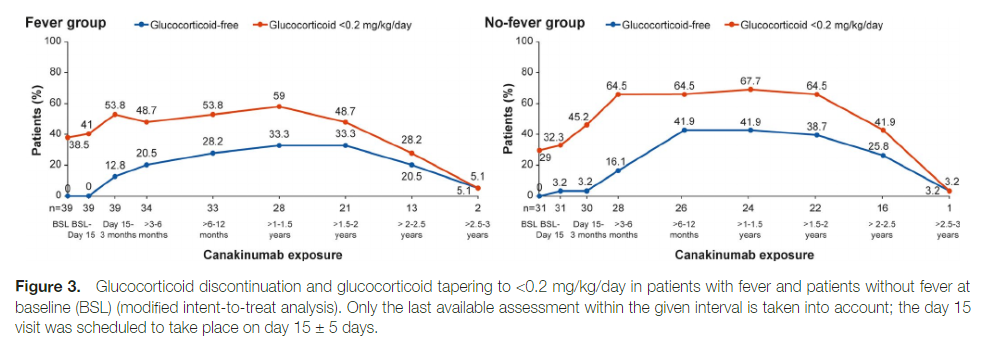
综上所述,该研究结果表明,无论治疗开始时是否有发热,卡那单抗都能快速、持续地改善活动性JIA。
原始出处:
Hermine I Brunner, et al., Efficacy and Safety of Canakinumab in Patients With Systemic Juvenile Idiopathic Arthritis With and Without Fever at Baseline: Results From an Open-Label, Active-Treatment Extension Study. Arthritis Rheumatol. 2020 Dec;72(12):2147-2158. doi: 10.1002/art.41436.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#特发性#
35
#系统性#
22
#Arthritis#
33
#关节炎#
31
#ART#
31
#卡那单抗#
42