Cell Death Differ:ARRB1和ARRB2在小胶质细胞介导炎症反应和帕金森病中表现出相反功能
2021-03-11 xiaozeng MedSci原创
帕金森病(PD)是仅次于阿尔茨海默病(AD)的第二大最常见的神经退行性疾病,其会影响2-3%的65岁以上的全球人群。
帕金森病(PD)是仅次于阿尔茨海默病(AD)的第二大最常见的神经退行性疾病,其会影响2-3%的65岁以上的全球人群。尽管目前尚未完全了解PD的发病病因和致病机制,但既往研究已显示,多种遗传因素和环境的暴露可导致PD的进展,这些可能的机制包括多巴胺代谢、线粒体功能障碍、内质网应激的变化、细胞自噬作用受损以及免疫力的降低。
小胶质细胞是大脑的主要免疫细胞,目前已有研究证实其与PD中激活的炎症反应相关。因此,鉴定涉及小胶质细胞活性的调节因子可为治疗PD的药物设计提供新的可能。
既往研究证实ARRB(β-arrestin)在中枢神经系统疾病的发病机制中具有不同作用。尽管ARRB能够调节多种生理和病理过程,但其在PD中的功能和调节作用仍不清楚。
在该研究中,研究人员发现,在PD小鼠模型中,特别是在小胶质细胞中,ARRB1(β-arrestin1)和ARRB2(β-arrestin2)的表达受到了相互调节。敲除ARRB1会改善PD的病理特征,包括体内多巴胺能神经元的丢失、神经炎症和小胶质细胞的激活、以及小胶质细胞介导的神经元损伤,而敲除ARRB2则会加剧相关病理特征。
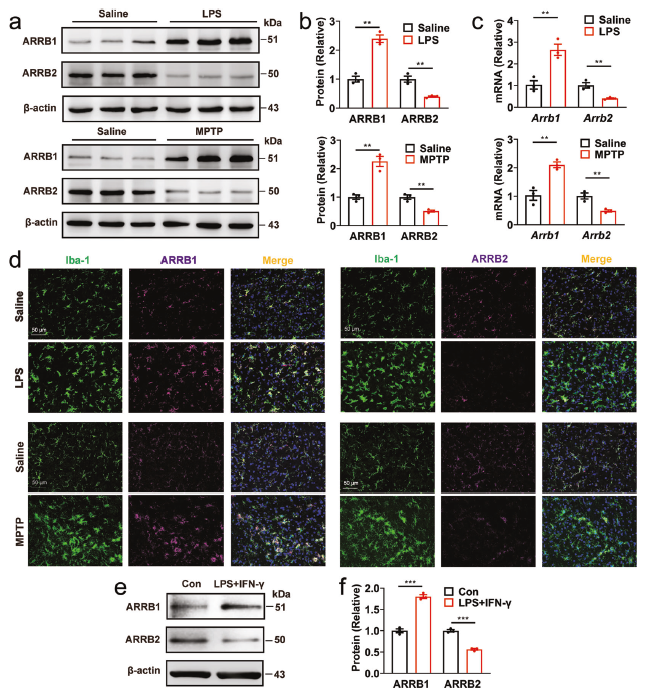
在PD小鼠模型中ARRB1和ARRB2的表达
研究人员发现,在原代培养的小胶质细胞和巨噬细胞中,ARRB1和ARRB2对炎症反应和炎性STAT1和NF-κB通路的激活产生不利的影响,且两种ARRB蛋白能够竞争性地与p65(NF-κB信号通路的成员之一)的活化形式相互作用。
进一步的研究显示,ARRB1和ARRB2能够差异性地调节Nprl3的表达,如RNA测序结果,在功能获得和丧失的研究中,Nprl3可以调节两个ARRB蛋白在小胶质细胞炎症反应中的功能。
相关原理图
总而言之,该研究结果显示,两种紧密相关的ARRB在小胶质细胞介导的炎症反应和PD的发病机制中发挥着相反的功能,这些功能部分由Nprl3所介导。该研究也为PD中ARRB的功能差异提供了新颖的见解。
原始出处:
Fang, Y., Jiang, Q., Li, S. et al. Opposing functions of β-arrestin 1 and 2 in Parkinson’s disease via microglia inflammation and Nprl3. Cell Death Differ (08 March 2021).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Differ#
39
#Cell#
53
努力学习中
67
#CEL#
40
#炎症反应#
48
#胶质细胞#
35
#Death#
35