Prostate Cancer P D:静脉麻醉下经直肠与经会阴前列腺活检比较分析
2020-08-23 AlexYang MedSci原创
经直肠(TR)和经肛门(TP)的前列腺活检方法具有不同的发病率。研究人员所在机构自2014年起转变倾向于基于MRI的多参数分诊和TP活检。最近,他们比较了TR和TP前列腺活检的临床、微生物学和健康经济
经直肠(TR)和经肛门(TP)的前列腺活检方法具有不同的发病率。研究人员所在机构自2014年起转变倾向于基于MRI的多参数分诊和TP活检。最近,他们比较了TR和TP前列腺活检的临床、微生物学和健康经济结果情况。
研究是一个连续的队列研究,包括了11年的前列腺活检。研究人员共进行了2048例前列腺活检。
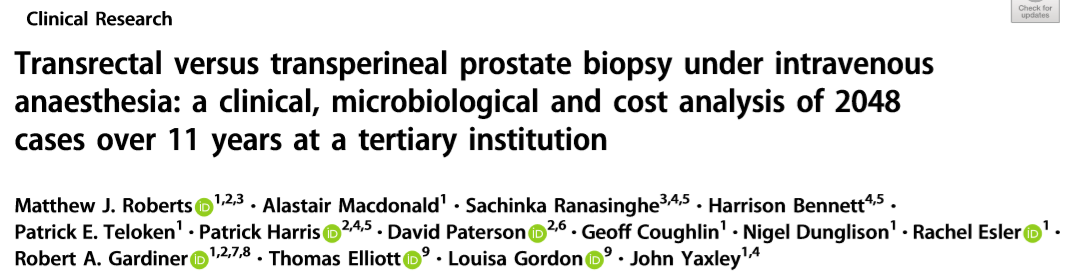
研究期间(2006-2017)进行的前列腺活检
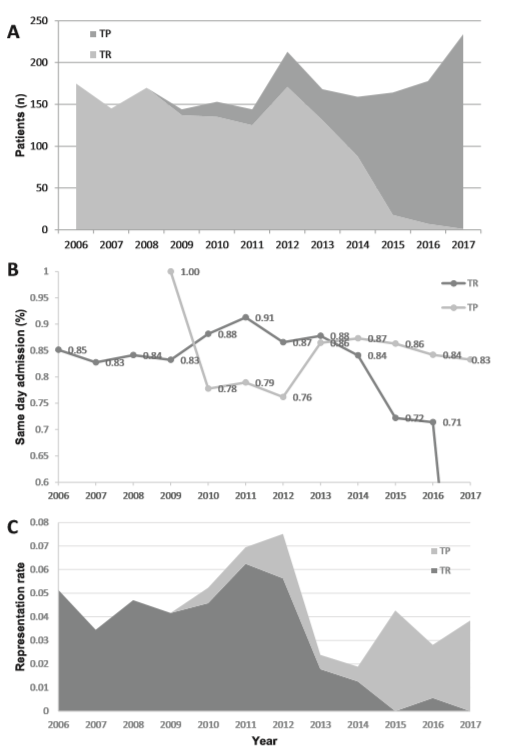
研究发现,每种活检方法的再次报告率相似(90名患者,TR 4.8%,TP 3.8%,p=0.29),其中23名患者再次报告一次以上(共119次重现)。TR活检后的报告更有可能是因为感染性病因(TR 2.92%,TP 0.26%新发,p<0.001),并导致入院(TR 43/49,93.4%;TP 14/24,58.3%;p=0.007),且尿潴留率相似(TR 2.76% vs TP 3.63%,p=1)。
再次报告和住院率信息
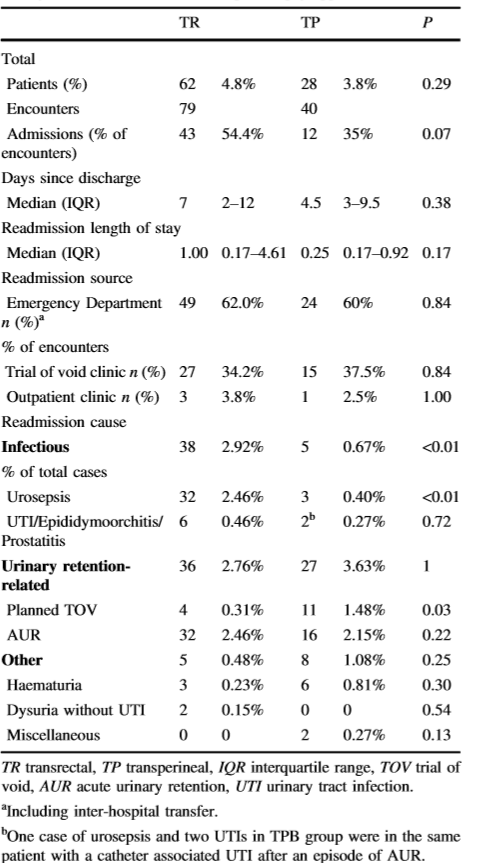
另外,调整了年数和年龄后,TP组的平均总费用(活检和再次报告)较高(p<0.001),但随着时间而降低,并且与再次报告的患者相似(p=0.98)。纳入mpMRI(随后避免活检)、TP活检和再次报告,每次活检可节省783.27澳元。
前列腺活检花费分析
最后,研究人员指出,在相似的再次报告率和尿潴留率下,TR活检比TP活检具有更多的感染性并发症和住院率。TP活检费用随着时间的推移而降低,与mpMRI联用可节约总体费用。另外,常规TP活检是安全可行的,与其他方法(局部麻醉)联用有望进一步节约成本,但仍旧在调查中。
原始出处:
Matthew J. Roberts, Alastair Macdonald, Sachinka Ranasinghe et al. Transrectal versus transperineal prostate biopsy under intravenous anaesthesia: a clinical, microbiological and cost analysis of 2048 cases over 11 years at a tertiary institution. Prostate Cancer P D. August 2020
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Prostate Ca#
37
#静脉麻醉#
38
#静脉#
36
#前列腺活检#
38
#比较分析#
28
学习了
83
#活检#
23
#ROS#
25
#会阴#
44
#PRO#
23