BMC: 肠粘膜中IL-12表达增加与溃疡性结肠炎的复发有关
2021-03-24 MedSci原创 MedSci原创
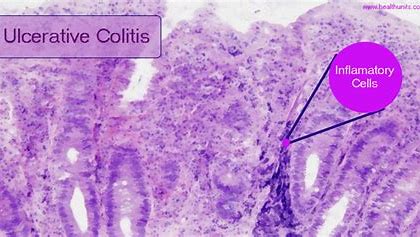
炎症性肠病(IBD)是包括溃疡性结肠炎(UC)和克罗恩氏病(CD)的一种慢性病,其特征是肠道反复出现炎症。
炎症性肠病(IBD)是包括溃疡性结肠炎(UC)和克罗恩氏病(CD)的一种慢性病,其特征是肠道反复出现炎症。免疫细胞(如T辅助细胞)和细胞因子(如白介素)都参与了疾病的发病。由于炎症介质与IBD的发病机理有关,因此这些分子已被用作其治疗的治疗靶标。TNF-α是第一个被确定为控制IBD的治疗靶标的分子,许多TNF-α抑制剂已被临床批准用于CD和UC的治疗。目前,另外一个细胞因子IL-12的促炎作用得到了越来越多的重视,IL-12首先被鉴定为促进干扰素(IFN)-γ产生的天然杀伤细胞刺激因子(NKSF)。有报道说,接受结直肠手术的UC患者发炎的黏膜中IL-12 mRNA表达显着升高,在本研究中,研究人员调查了粘膜IL-12表达与UC患者临床结局之间的关联。

研究人员从70例临床缓解的UC患者中收集直肠活检。通过实时荧光定量PCR测量IL-12,IL-23,IFN-γ,IL-17A和IL-17F mRNA的表达。内窥镜检查的严重程度和组织学活性分别通过Mayo内窥镜评分(MES)和Geboes评分进行评估。

本项研究中最长的随访期为51个月,在研究期间有34名患者复发。这些后来复发的患者的样品组成“复发”组,而那些未复发的患者的样品组成“缓解”组。 复发组中IL-12(P = 0.0003)和IL-23(P = 0.014)mRNA表达显着高于缓解组。IL-23(P = 0.015)而不是IL-12(P = 0.374)的表达与MES评分相关。但是,在MES为0和1的患者中,IL-12在复发中的表达在统计学上高于缓解组(P = 0.0015,P = 0.0342)。但是在缓解组中无组织学活动的患者两者均较高(IL-12:P=0.0002,IL-23:P = 0.046)。

本项研究发现在复发的UC患者中,患者的直肠粘膜中IL-12和IL-23表达均升高,但是无论内窥镜检查的严重程度和组织学活性如何,IL-12与UC复发的相关性更高。因此,研究人员说道IL-12在UC发病与复发中有着重要的作用。
原始出处:
Kazuhiko Uchiyama. Et al. Increased mucosal IL-12 expression is associated with relapse of ulcerative colitis. BMC Gastroenterology.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#溃疡性#
35
#IL-12#
29
#BMC#
26
#粘膜#
25
#IL-1#
32