STTT:国内多中心研究ORIENT-4证实PD-1抑制剂sintilimab(信迪利单抗)对有复发/难治性结外NK/T细胞淋巴瘤(r/r ENKTL)患者有效且耐受性良好
2021-12-29 yd2015 MedSci原创
ORIENT-4研究表明PD-1抑制剂sintilimab(信迪利单抗)对有复发/难治性结外NK/T细胞淋巴瘤(r/r ENKTL)患者有效且耐受性良好。
结外自然杀伤(NK)/T细胞淋巴瘤(ENKTL)是一种高度侵袭性的非霍奇金淋巴瘤(NHL)亚型,在亚洲和拉丁美洲发病率较高。在中国,ENKTL占所有NHL的6.6%,外周T淋巴瘤(PTCLs)的28.1%。ENKTL患者的5年总生存期(OS)为40-50%。Epstein Barr病毒(EBV)感染是ENKTL的重要病因和预后因素。EBV感染诱导的PD-L1过表达是ENKTL逃避免疫监测的潜在机制,而抗PD-1抗体在复发/难耐(r/r) ENKTL患者中显示出潜在的疗效。两项样本量有限的回顾性研究表明,pembrolizumab对r/r ENKTL有效,ORR为100% (n=7)和57.1% (n=7)。PD-L1抑制剂avelumab单药治疗r/r ENKTL时ORR为38%,CR率为24%。目前PD-1抑制剂在r/r ENKTL患者中的疗效尚不明确。因此,国内多家医院联合开展了多中心、单臂II期研究ORIENT-4 (NCT03228836),评估PD-1抑制剂sintilimab(信迪利单抗)治疗复发/难治性结外NK/T细胞淋巴瘤(r/r ENKTL)患者的疗效和安全性。相关结果发表在Signal Transduction and Targeted Therapy杂志上。
ORIENT-4是一项多中心、单臂、2期临床试验(NCT03228836)。患者至少接受一种天门冬酰胺为基础的治疗方案后进展,纳入患者接受200mg 信迪利单抗,每3周静脉注射一次,持续24个月。主要终点为客观缓解率(ORR)。
2017年8月31日至2018年2月7日,筛查34例患者,最终入组28例患者。中位年龄37岁(19-65岁),男性17岁(60.7%)。19例(67.9%)患者为IV期,25例(89.3%)患者ECOG PS为1和2。22例(78.6%)患者既往接受过放疗,2例(7.1%)患者接受过自体干细胞移植。
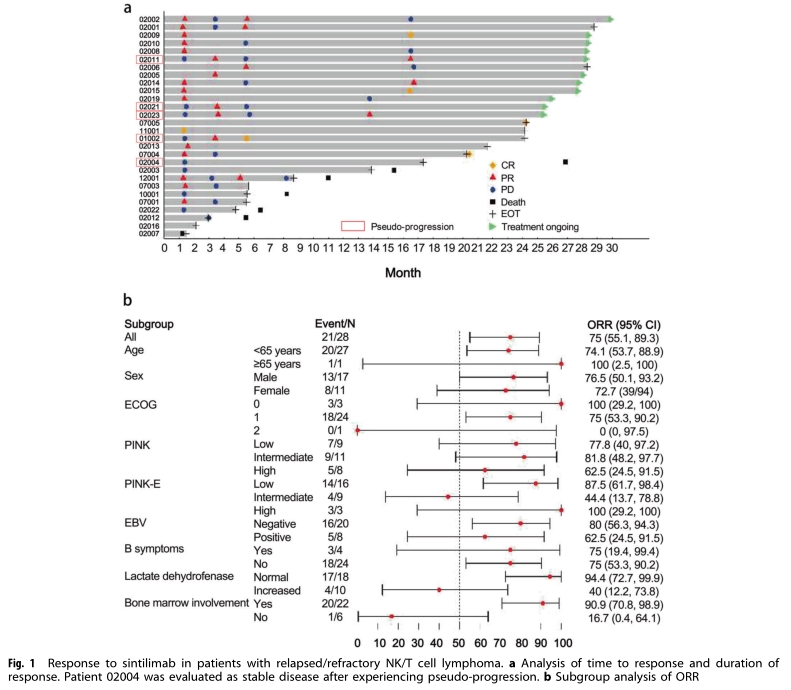
截至2020年2月28日,中位随访时间为30.4个月(范围:27.5-31.9个月)。中位治疗持续时间为24.2个月(范围:1.4 33.3个月), ORR (n = 21)实际上为75.0%(95%CI: 55.1-89.3)。CR和PR分别为21.4和53.6%。疾病控制率(DCR)为85.7% (95% CI: 67.3–96.0%)。中位缓解时间(TTR)为1.3个月(95% CI: 1.3-3.4),中位缓解持续时间(DOR)为4.1个月(95% CI: 2.1-15.2)。亚组分析显示,正常LDH(LDH, n=18, ORR=94.4%,95% CI: 65.3 98.6%)和骨髓未受侵犯(n =22, ORR=90.9%,95% CI: 59.7 94.8%)与更有利的ORR相关。
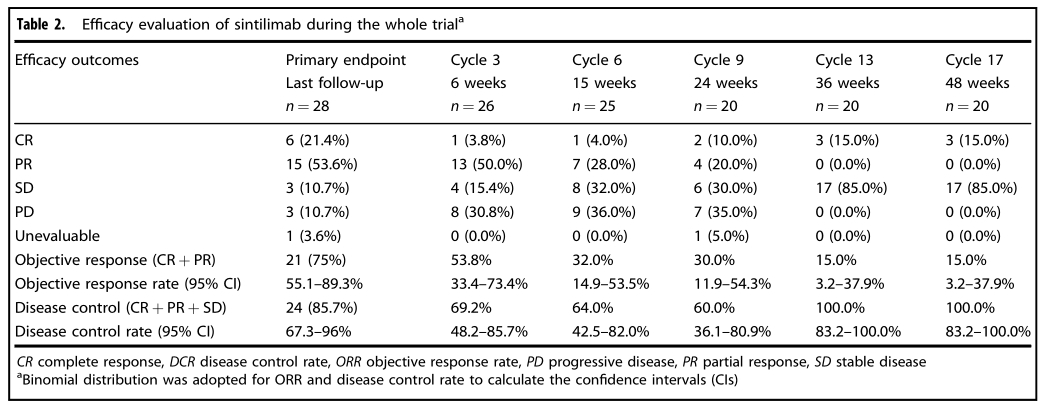
疗效评估
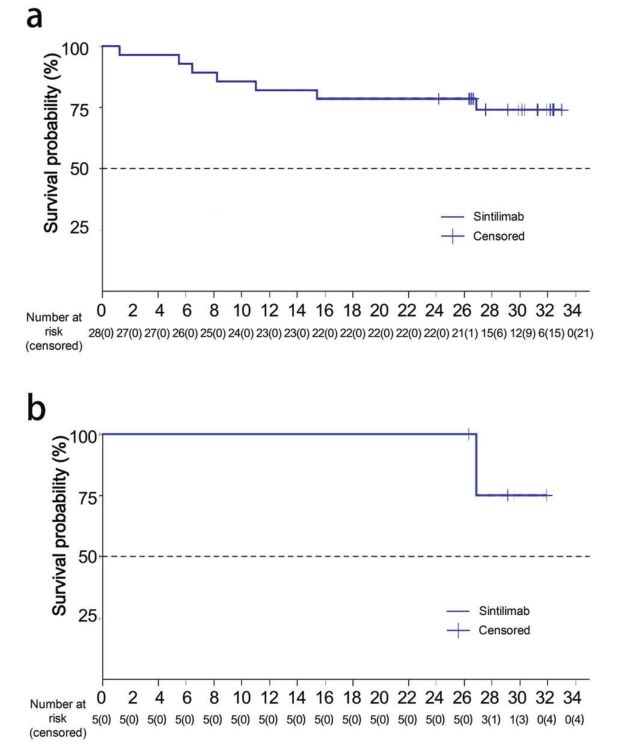
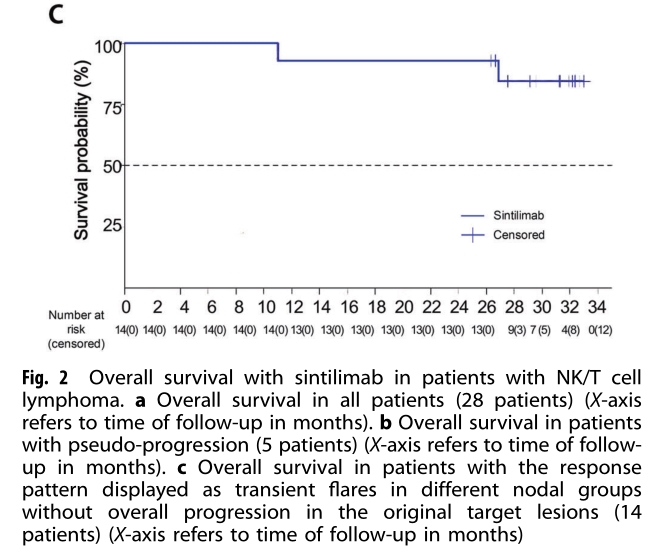
中位随访30.4个月,中位总生存期(OS)未达到。1年OS率为82.1% (95% CI: 62.3-92.1%), 2年OS率为78.6% (95% CI: 58.4-89.8%)。5例(17.9%)患者出现伪进展。在这些患者中,1年和2年OS率均为100.0% (95% CI: 100.0 100.0),中位OS未达到。14例(50.0%)患者,包括5例假进展患者,表现出一种模式,尽管出现新的病变但是无症状。在这些患者中,1年和2年的OS率均为92.9% (95% CI: 59.1-99.0%)。
预后分析
27例(96.4%)患者经历了至少一次治疗相关不良事件(TRAE),最常见的TRAE为淋巴细胞计数下降(46.5%)、发热(42.9%)和白细胞计数下降(35.7%)。大多数TRAE为1- 2级,只有1例患者出现4级TRAE(糖尿病)。无5级TRAE报告。7例(25.0%)患者报告了严重的AEs (SAEs),包括3级肺部感染、过敏性休克、急性胰腺炎、消化道出血、椎间盘疾病、局限性感染、酮症酸中毒。
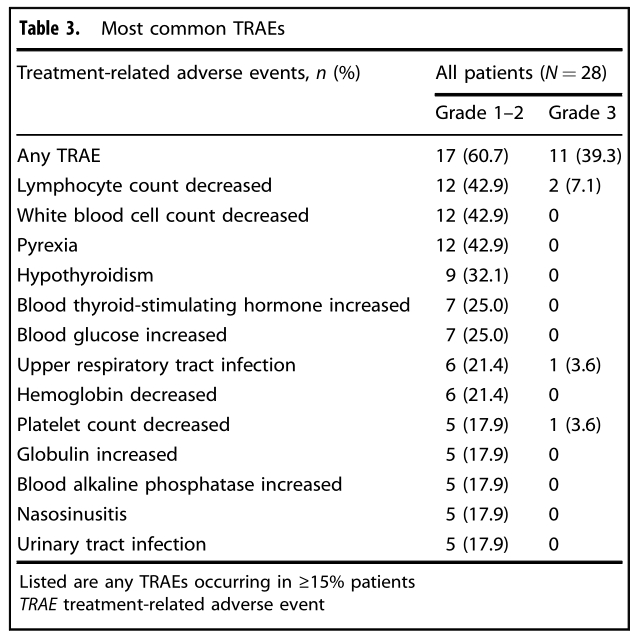
TRAEs
综上,ORIENT-4研究表明PD-1抑制剂sintilimab(信迪利单抗)对有复发/难治性结外NK/T细胞淋巴瘤(r/r ENKTL)患者有效且耐受性良好。
原始出处:
Tao R, Fan L, Song Y, Hu Y, Zhang W, Wang Y, Xu W, Li J. Sintilimab for relapsed/refractory extranodal NK/T cell lymphoma: a multicenter, single-arm, phase 2 trial (ORIENT-4). Signal Transduct Target Ther. 2021 Oct 27;6(1):365. doi: 10.1038/s41392-021-00768-0. PMID: 34702811; PMCID: PMC8548511.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言






#NK/T细胞淋巴瘤#
42
#抑制剂#
49
#NKT#
50
#细胞淋巴瘤#
43
#多中心研究#
44
#多中心#
37
#mAb#
32
#PD-1抑制剂#
35
#T细胞淋巴瘤#
54
#耐受性#
45