WICCVD 2016:胡盛寿——从医疗结果评价研究审视我国心血管外科临床实践几点思考和认知
2016-06-29 MedSci MedSci原创
2016年6月25日,由华中科技大学同济医学院附属协和医院主办的第三届武汉国际心血管病大会在武汉举行。在开幕式后的学术报告现场,本届大会主席、中国工程院院士,国家“973项目”首席科学家,中国医学科学院阜外心血管病医院院长胡盛寿院士做了关于我国心血管外科临床实践的学术报告,以下是详细内容:医改是一个世界性难题,无论是在美国和中国。各国政府的医改一直都积极以优化本国医疗体系为共同目标,其中,优化
2016年6月25日,由华中科技大学同济医学院附属协和医院主办的第三届武汉国际心血管病大会在武汉举行。在开幕式后的学术报告现场,本届大会主席、中国工程院院士,国家“973项目”首席科学家,中国医学科学院阜外心血管病医院院长胡盛寿院士做了关于我国心血管外科临床实践的医疗结果评价研究的学术报告,以下是详细内容:
医改是一个世界性难题,无论是在美国和中国。各国政府的医改一直都积极以优化本国医疗体系为共同目标,其中,优化医疗配置是医疗体系各层面共同面对的问题。
医改一直在进行,但是目前中国的医疗环境仍存在以下几点不足:
1.医疗资源配置不合理(政府补贴,城乡医疗投入等方面)
2.医疗结果和质量差异大(尤其是不同地区间的差异巨大)
3.医疗费用激增和医疗资源的浪费(在中国,60-70%冠脉介入指征失当)
那么,如何平衡医疗资源配置?如何缩小不同级别医院医疗质量差异和进行质量控制?医生为病人提供何种治疗最有效?行政部门确定多少费用是合理的?
解决上面这些问题就需要医疗结果评价研究的数据。医疗结果评价研究(Outcomes Research in Health Care),是对医疗体系中的各种政策的干预手段带给患者和服务对象的最终实际结果进行评价的应用型研究的统称(Science.1998)。它分为下面三类:
1.疗效对比研究(CER):通过比较研究确定最有效的治疗策略和方法
2.以患者为中心的结果评价研究(PCOR):研究确保所提供的医疗服务符合和尊重个体对象的需求与选择
3.医疗体系合理性评估:评价现有医疗体系构架的合理性并探讨改进的策略及途径
医疗结果评价研究的意义是重大的,如在心血管领域,通过Harlan Krumholz教授主导的临床结果评价,真正达到了提高冠心病二级预防普及的目的,且全美十年间急性心肌梗死死亡率下降了3%(由1995年的18.8%下降到了2006年的15.8%)!
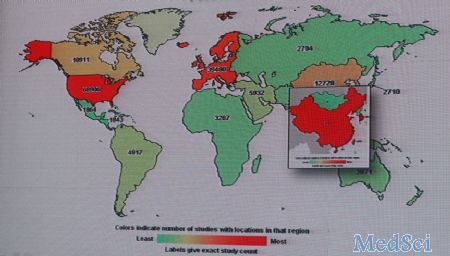
然而,在心血管领域,中国的原始创新心血管临床研究少。如下图所示,中国临床研究数量明显不足,仅占全球数目的2.7%,为美国的5.6%。
同时,中国临床评价体系的建设严重不足。如下图所示,是2001年-2010年间国内心血管临床研究发表情况,与欧美国家相比,国内临床评价体系建设不足,系统化数据缺乏,许多政策和指南更多地依赖了国外数据。

在报告中,胡盛寿院士为在场的国内外专家介绍了中国心血管外科注册登记研究的情况:
1.中国心血管外科注册登记研究是国内规模最大、覆盖面最广(30个省市的97个心脏中心,2014)的心血管外科专业数据库,累计收集病例14万例;
2.基于中国心血管外科注册登记研究,国人发现之前广泛使用的EuroSCORE并不能很好地预测国人手术风险,这都提示国人特殊性和建立个体化评估模型的必要性;
3.基于中国心血管外科注册登记研究的SinoSCORE大规模临床验证促进国际心血管外科风险评估模型的更新和改变,2011年EuroSCORE更新为EuroSCOREⅡ。
SinoSCORE能够准确评估国人冠心病外科风险,为手术策略的选择和个体化治疗提供依据,收益患者每年超过20000例。同时,通过中国心血管外科注册登记研究,发现规范化术前风险评估、治疗流程,强化临床疗效评估降低了手术死亡率和手术并发症的发生。
总结:中国医疗结果评价研究——中国心血管外科注册登记研究
1.CCSR医疗质量的提高
·注册登记患者预期寿命提高1岁
·每年用于CABG的医疗费用减少1.6千万
2.如果将CCSR的临床结果评价历年推广到全国
·全国CABG患者预期寿命提高1岁
·每年用于CABG的医疗费用减少8千万元
中国医疗结果评价研究,既促进了中国心血管外科临床实践的发展(如上),又推动了国际上对心血管外科临床的认识(详见附录),因此继续推动中国医疗结果评价研究是必需的。
目前的中国医疗结果评价研究亟需解决的问题是——建立心血管病防控数据库。中国心血管病防控数据库的建立不仅需要政府的大力导向、行政与专业部门的资金支持,更需要对专业人员进行专业的培训,以及群众宣教。
建立心血管病防控数据库体系将会为制定卫生政策和建立临床质量评价体系提供理论依据,实现临床指南和卫生政策转化。
附录:中国心血管外科注册登记研究的其它研究结果
1.左主干病变CABG与PCI疗效的对比研究(J Am Coll Cardiol Intv.2016;9[11]:1102-1111)发现:对于无保护左主干病变,接受CABG的患者随访期间死亡率及再干预率较低
2.体外与非体外CABG疗效对比研究(Circulation.2010;121:1800-1808)发现:非体外CABG患者远期MACCE和二次血运重建发生率明显增高。(研究结果被2011年美国ACCF/AHA冠脉搭桥指南引用。)
3.CABG+骨髓干细胞治疗的随机对照试验(J Am Coll Cardiol 2011;57:2409-15)证实:CABG+骨髓干细胞治疗对心梗后心衰患者心功能具有改善作用。(2013年ACCF/AHA心衰指南引用)
4.杂交技术和单纯CABG或PCI疗效对比研究(J Am Coll Cardiol 2013;61:2525-33)发现:对于多支病变患者,一站式杂交治疗获益明显,特别是对于EuroSCORE或SYNTAX score评分较高的患者。
5.CABG术后双抗和单抗血小板治疗的随机对照研究(J Am Coll Cardiol 2010;56:1639-43)发现:CABG术后阿司匹林和氯吡格雷联合抗血小板治疗和单纯阿司匹林治疗相比,静脉桥血管早期通畅率高。(被2012版美国STS心脏/非心脏手术患者抗血小板药物指南、2015版冠脉搭桥术后二级预防指南引用)
6.β受体阻滞剂对搭桥手术预后的影响研究(Circulation 2015;131:2194-2201)发现:搭桥术后持续使用β受体阻滞剂可以提高远期生存率。
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#胡盛寿#
35
牛人!
52
#心血管外科#
50
#临床实践#
34
#血管外科#
27
#评价#
21
#ICC#
33
学习力
99
中国心血管发展迅速
73
好好?!!!!!
88