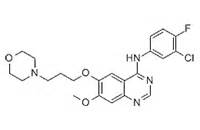
J Am Acad Dermatol:吉非替尼治疗难治性皮肤鳞状细胞癌的疗效如何?(单臂Ⅱ期临床试验)
2017-10-31 MedSci MedSci原创
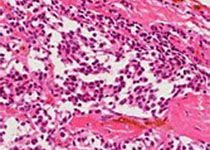
背景:临床前数据表明了表皮生长因子受体(epithelial growth factor receptor,EGFR)对皮肤鳞状细胞癌(cutaneous squamous cell carcinomas,CSCC)的发病起着关键性作用。EGFR本身具有酪氨酸激酶活性,一旦与表皮生长因子(EGF)组合可启动细胞核内的有关基因,从而促进细胞分裂增殖。胃癌、乳腺癌、膀胱癌和头颈部鳞癌的EGFR表达增高
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#细胞癌#
37
#ACA#
32
学习了谢谢作者分享!
67
好知识.值得拥有
70
#难治性#
35
不错的文章值得一读
66
学习了感谢分享
67