“安全阴云”笼罩肿瘤免疫疗法领域
2015-01-29 佚名 生物谷
癌症,一直是全世界科学家试图征服的对象。为此,人们先后开发了化疗、放疗等手段用来杀灭肿瘤细胞。然而,这些治疗方案要么是“威力”不够,无法抑制肿瘤细胞的疯狂生长;要么是伤敌一千,自损八百。 随着科学家对免疫系统的了解,科学家们开始意识到人类自身的免疫系统或许是最终解决这一问题的最好武器。2014年生物医药研究领域开始掀起了一场肿瘤免疫疗法的研究热潮。这其中最为耀眼的当属CAR-T疗法和双特异性
癌症,一直是全世界科学家试图征服的对象。为此,人们先后开发了化疗、放疗等手段用来杀灭肿瘤细胞。然而,这些治疗方案要么是“威力”不够,无法抑制肿瘤细胞的疯狂生长;要么是伤敌一千,自损八百。
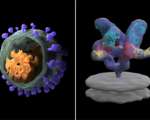
随着科学家对免疫系统的了解,科学家们开始意识到人类自身的免疫系统或许是最终解决这一问题的最好武器。2014年生物医药研究领域开始掀起了一场肿瘤免疫疗法的研究热潮。这其中最为耀眼的当属CAR-T疗法和双特异性抗体疗法。
CAR-T疗法是通过分离患者体内的T细胞,然后将这些T细胞通过基因工程的手段与特定的抗体片段相连,在体外进行扩增后回输至患者体内,进而特异性杀灭肿瘤细胞。因为这些T细胞来源于患者本身,从而避免了异源物质在体内引起的排斥反应。而双特异性抗体则是抗体研究的一个突破,传统的Y型抗体只能识别一种抗原。科学家们通过重组等方式,构建了这种双特异性抗体,使其能够靶向特定肿瘤细胞的同时还可以识别T细胞。这使得肿瘤细胞呈递至T细胞的效率大大增强,也使得免疫疗法的效果有了质的飞跃。治疗白血病的临床研究显示,有40%-90%的患者经过治疗后,甚至检测不到癌细胞的存在。如此好的治疗效果,无怪乎一些分析人士对未来肿瘤免疫市场规模给出了1000亿美元这一近乎天方夜谭的数字。而如果这些方案对于实体瘤治疗也有同样的效果,那么这一市场还将会继续扩大。
安全阴云笼罩肿瘤免疫疗法
说到这里,许多人或许觉得人类对抗癌症的前景似乎是一片大好,人类彻底治愈肿瘤的时候似乎已经为期不远。然而,一名合格的科学家应当是时刻保持理性的。就在肿瘤免疫疗法近乎被神话的时候,许多科学家纷纷开始正式这一疗法潜在的安全风险。
归结起来,这些免疫疗法的隐患主要集中于两点。
首先是这两种疗法突破了免疫系统的极限,使得T细胞以前所未有的超高效率识别和杀灭肿瘤细胞。通过T细胞体外扩增或是双特异性抗体使T细胞在肿瘤部位富集,免疫系统产生抗体的数量和速度要大大加快,这也是肿瘤细胞能在短时间内被杀灭的主要原因。然而,大量肿瘤细胞的死亡可能会导致肿瘤细胞内各种细胞因子被释放出来,这些细胞因子会在患者体内引起一系列连锁反应,并最终导致炎症、低血压等副作用,甚至导致患者死亡。
其次,以目前CAR-T疗法和双特异性抗体疗法研究最多的适应症--白血病--为例,大部分的免疫疗法都是以一种名为CD19的特异性蛋白为靶点。然而,这种蛋白在许多正常组织中都会有少量分布,因此,当T细胞在体内大量富集的时候,自身免疫的风险就会大大增加。同时,美国FDA的相关专家还表示,由于免疫疗法实际上是改变了体内的免疫系统平衡,因而很难判断造成这种副作用的确切原因是什么,这也是为什么一些传统的抑制自身免疫的方法在这一新兴疗法中不起作用的原因。不久前CAR-T疗法的先驱Juno公司相关产品临床研究中就出现两名患者非正常死亡的事件也为肿瘤免疫疗法的前景蒙上了一层阴影。
显然,许多生物医药公司也已经认识到了这一问题,一些CAR-T疗法研究人员为富集的T细胞添加了一个特殊的“自杀开关”,以确保这些T细胞在清除完目标后不会误伤健康组织。
肿瘤免疫疗法的前景
尽管肿瘤免疫疗法还面临着这样和那样的问题,但是这并不妨碍各方将其看作是癌症治疗的明日之星。目前,包括Juno公司、Kite公司、诺华公司和安进公司在内的各大生物医药巨头都全力以赴的开发CAR-T疗法,而辉瑞、强生和礼来公司等也正在开发超过三十种的双特异性抗体药物。有人估计,这些药物上市后的价格将高达30-50万美元。而就在上月,FDA已经批准了首个双特异性抗体药物--安进公司开发的Blincyt用于治疗急性粒细胞白血病。诺华公司的CAR-T疗法的临床研究也取得了令人瞩目的成果。
可以预见,肿瘤免疫疗法的兴起将会为整个医药产业带来一次重新洗牌的机会!
详细英文报道:
(Reuters) - A new wave of experimental cancer drugs that directly recruit the immune system's powerful T cells are proving to be immensely effective weapons against tumors, potentially transforming the $100 billion global market for drugs that fight the disease.
But top oncology researchers are concerned about the two emerging technologies, citing dangers seen repeatedly in clinical trials including the potentially fatal buildup of toxic debris from killed tumor cells and damage to healthy tissue. Such side effects could block regulatory approval if they aren't controlled, researchers and drug company executives said in interviews with Reuters.
In some trials, the two new approaches, known as CAR T cells and bispecific antibodies, have eliminated all traces of blood cancers in 40 percent to 90 percent of patients who had no remaining options. The drugs could reap annual sales in the tens of billions of dollars for their manufacturers, especially if they can also eliminate solid tumors in such terminally ill patients.
CAR T cells, or chimeric antigen receptor T cells, are T cells that have been removed from the body and attached through genetic engineering to an antibody fragment that recognizes a specific tumor protein. T cells are an especially powerful disease-fighting kind of white blood cell. The result is a drug with the killing power of a greatly enhanced T cell, combined with the tumor-spotting ability of an antibody.
Bispecific antibodies are a twist on conventional antibodies, Y-shaped proteins whose two arms grasp for the same protein target found on cancer cells.
With bispecifics, one arm of the antibody typically grasps a cancer cell while the other arm takes hold of T cells, bringing the mortal enemies into contact. The T cell punches holes into the adjacent tumor cell and injects deadly enzymes. Conventional antibodies, by contrast, don't directly recruit T cells.
"Unleashing the killing power of the T cell directly on the tumor cells allows a large increase in potency of these antibodies," said Dr. David Scheinberg, chairman of molecular pharmacology at Memorial Sloan Kettering Cancer Center.
Investor excitement over these therapies have helped boost interest from companies including Amgen Inc and Roche and have fueled a jump in share prices of smaller firms such as Kite Pharma Inc, Juno Therapeutics and Bluebird Bio.
"We take patients that have failed every treatment, every chemo combination, that have just two to six months to live. You give them a CAR, and within 3 to 4 weeks you can see massive tumors melting away," said Arie Belldegrun, chief executive officer of Kite. The company went public in June and announced a partnership with Amgen earlier this month.
CAR T cells could cost $300,000 to $500,000 per patient, if approved, making them among the world's most expensive drugs and testing the ability of insurers to pay for them, said Les Funtleyder of E Squared Asset Management. The hedge fund owns shares of Kite Pharma. Bispecific antibodies could command prices of $200,000 or higher, he said.
The potency of the experimental drugs comes with some dangerous potential side effects. In the killing process, inflammatory chemicals from the medicines and the tumor cells, called cytokines, are released into the bloodstream and can cause fever, low blood pressure and rapid heartbeat that can be life-threatening.
The drugs, because of their unique structure and how they work, make it harder to predict whether they will go astray, said Dr. Bindu George, team leader of the U.S. Food and Drug Administration's Office of Cellular, Tissue and Gene Therapies, who called CAR T drugs perhaps the most interesting new technology.
Most CAR T cells and bispecific antibodies in development identify blood cancer cells by a specific protein, CD19, found on the surfaces of lymphomas and leukemias. Because the same protein can also be found on non-cancerous cells, the drugs can go off track and attack healthy tissues.
"Our biggest concern would be an off-target toxicity that wasn't expected and we didn't know the cause of it," George said. In that case, "we might have to ask (the drugmaker) for additional information, how the toxicity happened, what organ it was, and literally go back to the drawing board."
TAMING A POWERFUL DRUG
Researchers have used anti-inflammation medications to tame some of the adverse reactions, not always successfully. A study of CAR T cell treatment sponsored by Juno for patients with aggressive non-Hodgkin's lymphoma was briefly put on hold after two people died.
Unlike antibodies, which are excreted from the body within days or weeks, engineered CAR T cells are expected to circulate for years or even a lifetime in the bloodstream, potentially providing lasting benefits, but also risks.
"You can start to reject normal tissues; it can kill organs or cause autoimmune disease, and you don't want that," said Zelig Eshhar, a professor emeritus of the Weizmann Institute in Israel who pioneered the CAR approach.
To reduce that danger, researchers are attempting to build "suicide switches" into CAR T cells to turn them off after they have wiped out all signs of cancer.
At least 30 bispecific antibodies are believed to be in development, including ones from Roche, Johnson & Johnson, AbbVie and Eli Lilly.
A growing number of drugmakers are also racing to develop the first CAR T therapies, including Kite, Novartis, Juno, Cellectis and its partner Pfizer Inc, and Bluebird, in partnership with Celgene Corp.
EXPENSIVE OPTION
The FDA in December approved the first bispecific, Amgen's $178,000 Blincyto for acute lymphoblastic leukemia (ALL) that did not respond to previous treatment. The cancer, prevalent in children, is diagnosed each year in an estimated 6,020 Americans, killing about a fourth of them.
One third of patients in the Amgen study had no detectable cancer for nearly seven months after receiving the drug through a month-long infusion.
A main hope for Blincyto is that it will keep patients alive until they can receive stem cell transplants, their best chance of a possible cure.
CAR technology may also come to the rescue where few options remain.
"If doctors and specialists learn how to control this very powerful gun, CAR T cells could save hundreds of thousands of people in the United States," said Ori Hershkowitz, a Tel Aviv-based fund manager with Sphera Funds, which owns shares of Kite and rival CARs developer Novartis.
A Novartis trial showed 27 of 30 children and adults with ALL had no signs of the disease after being treated with its CAR T drug. Some 78 percent of patients were still alive six months after treatment, while some sustained remission for up to two years.
But everyone in the study developed cytokine release syndrome, including a severe form of it in 27 percent of patients.
"It certainly needs to be watched and evaluated," said Usman Azam, global head of cell therapies for Novartis. He still believes the drug's benefits provide "compelling hope that you can potentially cure patients."
Roche's Genentech unit is conducting a mid-stage trial of a bispecific antibody to treat head and neck cancer and colorectal cancer. It is studying a dozen others in preclinical trials against cancer, Alzheimer's disease and inflammatory diseases.
Paul Carter, a Genentech executive, was cautious about the prospects.
"It's too early to say whether this will be a home run, although there's optimism it will be at least a base hit that will help us figure out how to go further."
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#肿瘤免疫疗法#
46