PRS:四氯十氧阴离子(TCDO)复合物滴注负压伤口疗法加速伤口愈合
2021-08-23 MedSci原创 MedSci原创
负压伤口疗法(NPWT)可促进肉芽组织的形成,增加局部血流量,减少组织水肿和清除渗出物,是一项标准的加速伤口愈合的方法。局部创面溶液滴注NPWT的结合为创面愈合提供了进一步的好处。
负压伤口疗法(NPWT)可促进肉芽组织的形成,增加局部血流量,减少组织水肿和清除渗出物,是一项标准的加速伤口愈合的方法。局部创面溶液滴注NPWT的结合为创面愈合提供了进一步的好处。
既往的研究表明TCDO可显著降低糖尿病足溃疡伤口的严重程度评分、感染、炎症和坏死组织的形成,从而促进肉芽组织的形成。
该前瞻性随机对照试验临床研究文章发表于2021年8月刊prs。按照伤口面积≥4cm2、伤口深度≥10mm、创面愈合时间预计≥15天等标准,最终纳入48名成年患者。
这项研究旨在于比较NPWTi(TCDO滴注+负压伤口疗法)与NPWT(标准负压伤口疗法)的疗效区别。
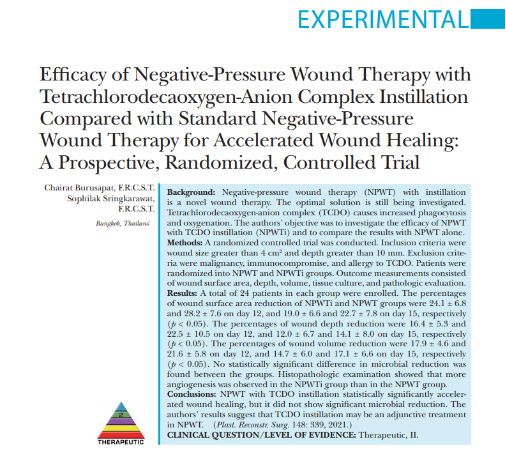
图1.来源截图
在研究前,研究人员对患者进行TCDO溶液皮肤过敏试验后,采用连续15天的负压伤口疗法治疗。两组的负压均设置为-125 mmHg,均每3天更换一次敷料。
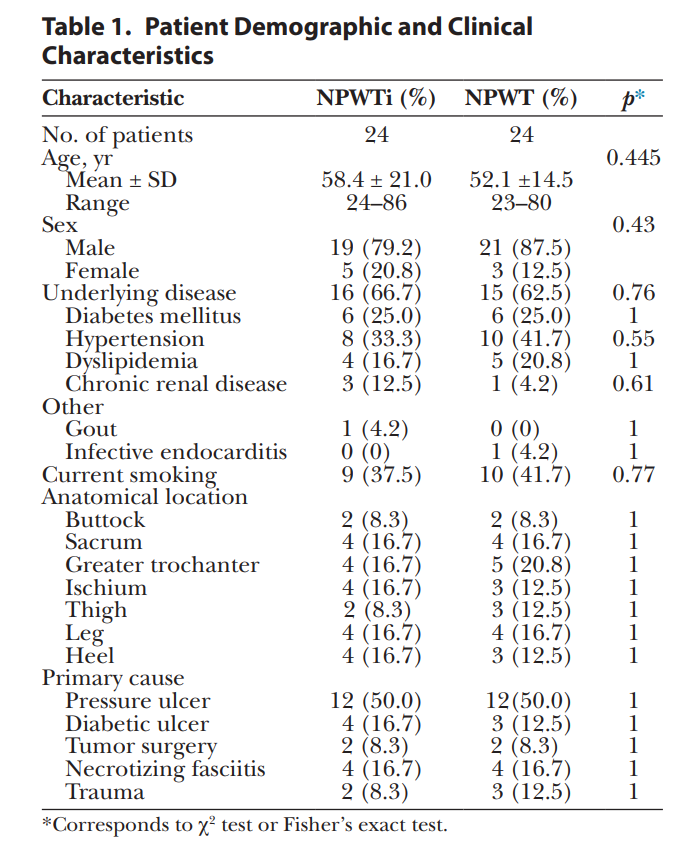
两组患者之间年龄、性别、基础疾病、当前吸烟情况与否、创面的解剖位置、原因和伤口手术次数均没有统计学差异。
这些患者的创面分别来源于截瘫患者的压疮、糖尿病足部溃疡、创伤后的伤口、坏死性筋膜炎和肿瘤手术术后复杂的创面缺损伴皮瓣重建失败情况。
表1 患者特征
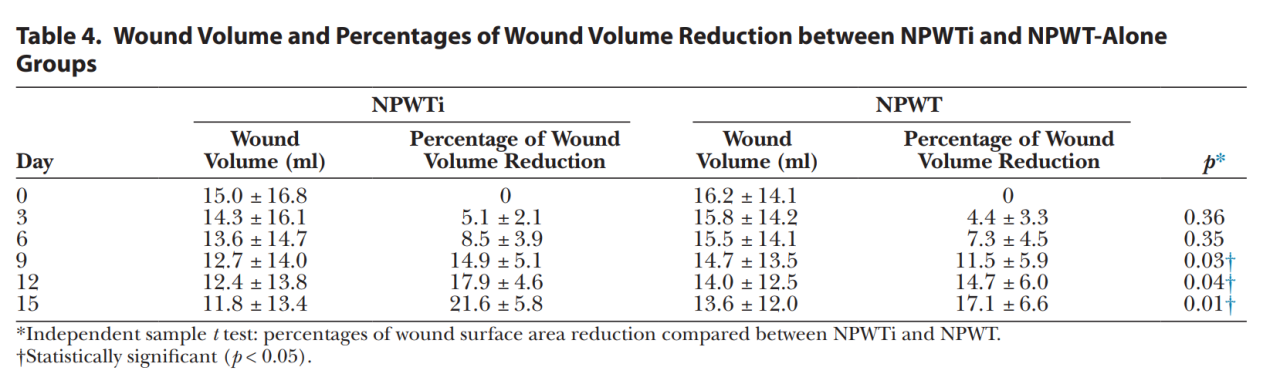
结果表明,TCDO复合灌注负压创面疗法在伤口表面积、深度和体积方面显著加速伤口愈合。
表2 创面面积及缩小程度
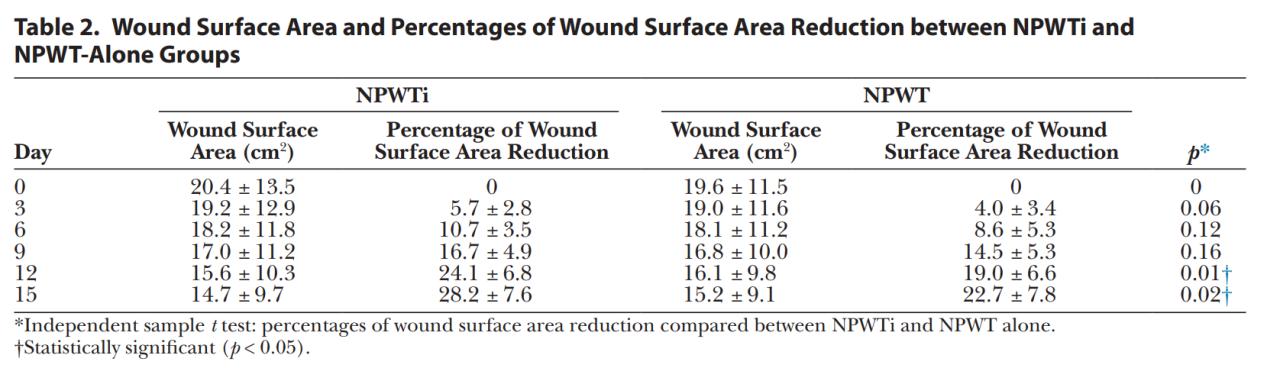
表3 创面深度及降低程度

表4创面体积及减小程度
组织学培养结果显示,两组均没有明显的规律改变,两组之间也没有统计学差异。组织病理学结果显示,NPWT组较NPETi组的新生毛细血管数量更少,水肿的间质细胞更多。
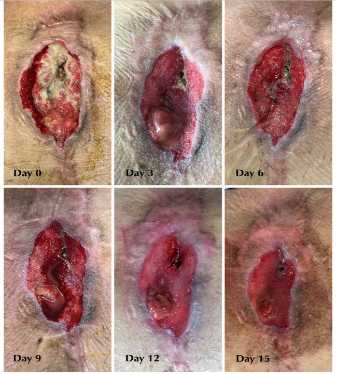
图2 伤口大小的改变情况图
研究结果表明,TCDO复合灌注负压创面疗法在伤口表面积、深度和体积方面显著加速伤口愈合。而在NPWTi组和单独NPWT组之间,细菌减少没有统计学上的显著差异。
将TCDO与NPWT结合使用主要是为了消除微生物,但NPWTi对细菌减少的益处尚不确定。虽然NPWTi的益处已经得到证明,但注入的解决方案仍不确定。
a.TCDO灌注的最佳停留时间:既往研究的适当范围在10-20分钟
b.TCDO的最佳灌注频率:既往研究为2-24次每天
c.TCDO的最佳灌注量:观察泡沫的饱和度
因此,研究人员认为,TCDO灌注在标准负压创面治疗中可作为一种辅助治疗。
原始文献:
Burusapat Chairat,Sringkarawat Sophilak,Efficacy of Negative-Pressure Wound Therapy with Tetrachloro decaoxygen-Anion Complex Instillation Compared with Standard Negative-Pressure Wound Therapy for Accelerated Wound Healing: A Prospective, Randomized, Controlled Trial.[J] .Plast Reconstr Surg, 2021, undefined: undefined.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TCD#
0
#复合物#
37
好文章
46
#PRS#
36
#伤口愈合#
44