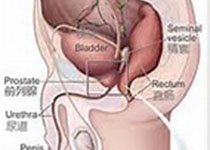
Prostate Cancer P D:下尿路症状对死亡率的影响
2018-11-16 AlexYang MedSci原创
下尿路症状(LUTS)作为死亡率风险因素的使用情况仍旧不清楚。考虑到症状的波动和症状的重新复发,重复性的评估师需要的。最近,有研究人员在中年和老年男性中,评估了与3种尿路储存相关的死亡率,包括紧急情况,白天尿频和夜尿情况,同时也考虑了跟踪调查期间,其他的随时间变化的因素。研究人员在芬兰进行了基于群体的通信调查,时间分别为 1994, 1999, 2004和2009年,跟踪调查起始年龄分别为50、6
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#尿路症状#
39
#Prostate Ca#
24
#下尿路#
38
#ROS#
21
#下尿路症状#
45
#PRO#
26
学习了谢谢分享
51