IDSA:A组链球菌性咽炎临床指南更新
2012-10-08 夏沫 中国医学论坛报
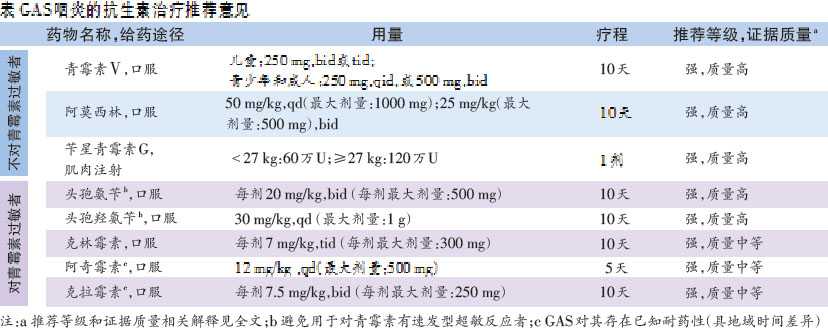
9月9日,美国感染病学会(IDSA)发布A组链球菌(GAS)咽炎诊断和管理指南,对2002年指南进行了更新。 该指南对GAS的诊断和治疗进行了讨论,并就抗生素选择和剂量提供了相关推荐意见(下表)。指南全文发表于《临床感染性疾病》(Clin Infect Dis)杂志。
9月9日,美国感染病学会(IDSA)发布A组链球菌(GAS)咽炎诊断和管理指南,对2002年指南进行了更新。
该指南对GAS的诊断和治疗进行了讨论,并就抗生素选择和剂量提供了相关推荐意见(下表)。指南全文发表于《临床感染性疾病》(Clin Infect Dis)杂志。

小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#指南更新#
32
#临床指南#
36
#咽炎#
35
#DSA#
25
#IDSA#
31
#链球菌#
32