抗肿瘤血管生成可能是脑胶质瘤治疗途径之一
2013-07-19 驻地记者张献怀 中国医学论坛报
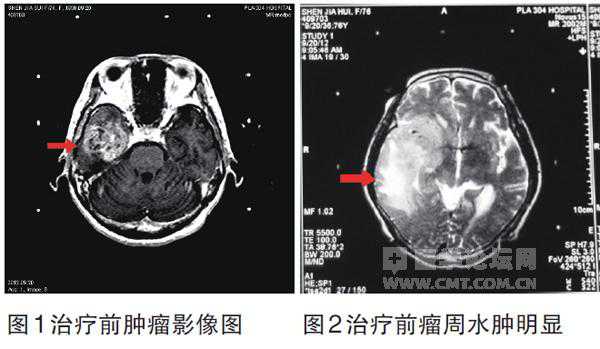
76岁的姜女士患脑胶质瘤已无条件手术,解放军总医院第一附属医院神经外科,采用抗血管生成靶向疗法对其进行治疗,取得良好效果,肿瘤明显缩小,瘤周水肿消退,患者自觉症状消失。据该科主任张志文介绍,这是他们采用该技术治疗的第27例患者。 该患者2012年9月突然感觉左侧肢体无力
 |
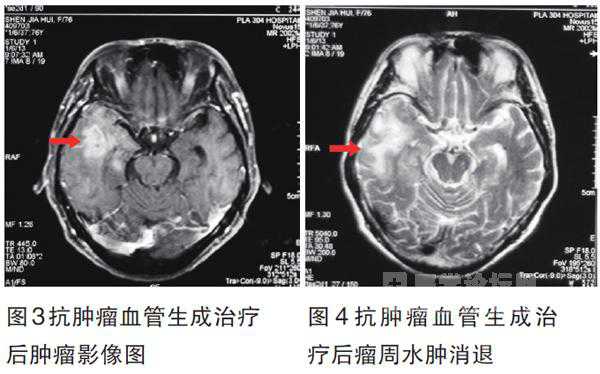 |
76岁的姜女士患脑胶质瘤已无条件手术,解放军总医院第一附属医院神经外科,采用抗血管生成靶向疗法对其进行治疗,取得良好效果,肿瘤明显缩小,瘤周水肿消退,患者自觉症状消失。据该科主任张志文介绍,这是他们采用该技术治疗的第27例患者。
该患者2012年9月突然感觉左侧肢体无力,走路不稳,有时跌倒,到医院检查发现,右颞部有一直径6 cm左右的占位,诊断为恶性脑胶质瘤。张志文等对患者病情及身体状况进行综合分析评估,认为根据病情应首选手术治疗,但患者有10余年的高血压和心血管病史,同时伴糖尿病,加上年龄较大,手术风险很大。患者本人也表示不愿意接受手术治疗。经多次讨论并与患者沟通,他们决定采用抗肿瘤血管生成靶向疗法为其进行治疗。经2次治疗后,磁共振复查,原肿瘤明显缩小,且基本无强化效应,瘤周水肿也明显消退,说明肿瘤已大部坏死,患者自觉头晕、肢体无力等症状消失,已于近日出院。
张志文介绍说,该技术2009年通过美国食品与药物监管局批准并应用于恶性脑瘤治疗,取得良好效果。抗血管生成靶向疗法适用于脑恶性肿瘤,尤其对术后复发、部位特殊、或因年迈体弱身体条件差等原因而不能手术的患者,开辟了一条新的治疗途径。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#肿瘤血管#
38
#抗肿瘤血管生成#
33
#肿瘤血管生成#
33