JACC:血管钙化会加速相关心血管事件进展吗?
2016-01-05 崔倩 译 MedSci原创
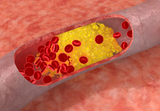
动脉粥样硬化是一种在疾病过程中有明显钙化的炎症状态。冠状动脉钙化的程度和进展可预测心血管事件。相对鲜为人知的是非冠状动脉血管钙化。这项研究调查非冠状动脉血管钙化和其对于血管炎症变化的影响。在dal-PLAQUE(dalcetrapib对于动脉粥样硬化性疾病的安全和疗效,采用新型非侵入性的多模态成像完成)研究中共有130名参与者,这些参与者在招募时和招募后6个月时进行了氟正电子发射断层扫描/计算机断
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#血管事件#
31
#JACC#
26
这篇文章有一定深度
93
是一篇不错的文章
161
这个值得关注
104
#ACC#
24
值得关注
22
赞一个
153
钙化与心血管疾病的发生关系很密切的
83
有意思
42