74岁,女性。
因眩晕和姿势不稳6个月,急性恶化。
MRI 显示小脑和脑干急性梗死。神经血管评估显示严重的血管损伤,沿椎基底动脉可见多处狭窄和闭塞(图1)。
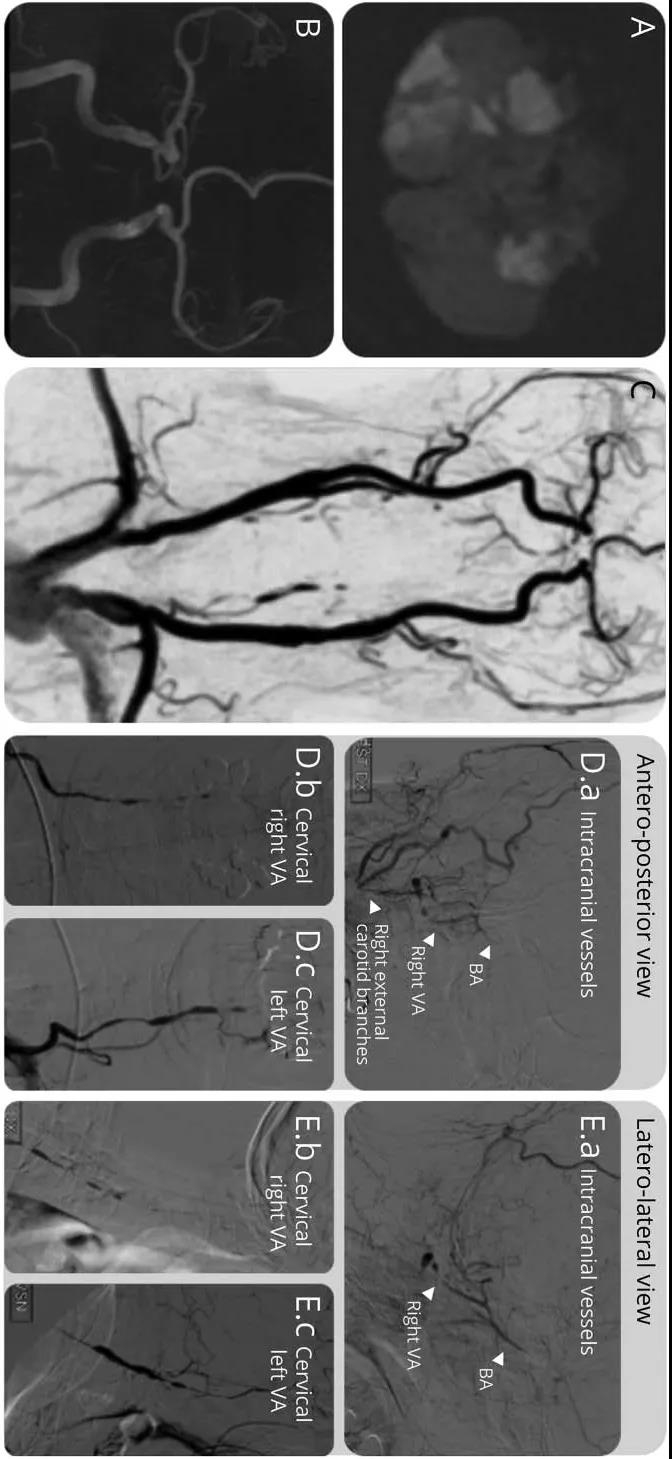
图1.DWI显示小脑梗死(A)。TOF MRA可见左椎动脉和基底动脉未显影(B)。对比增强MRA显示颅外椎动脉闭塞、颅内椎动脉和基底动脉规则(C)。DSA显示右侧颈外动脉和椎动脉之间的侧支循环(D.a–E.c)。
多普勒超声显示沿面动脉的低回声晕征,而PET-CT显示沿椎动脉和其他较大动脉可见氟-18-氟脱氧葡萄糖摄取增加,因此诊断为巨细胞动脉炎(图2)。
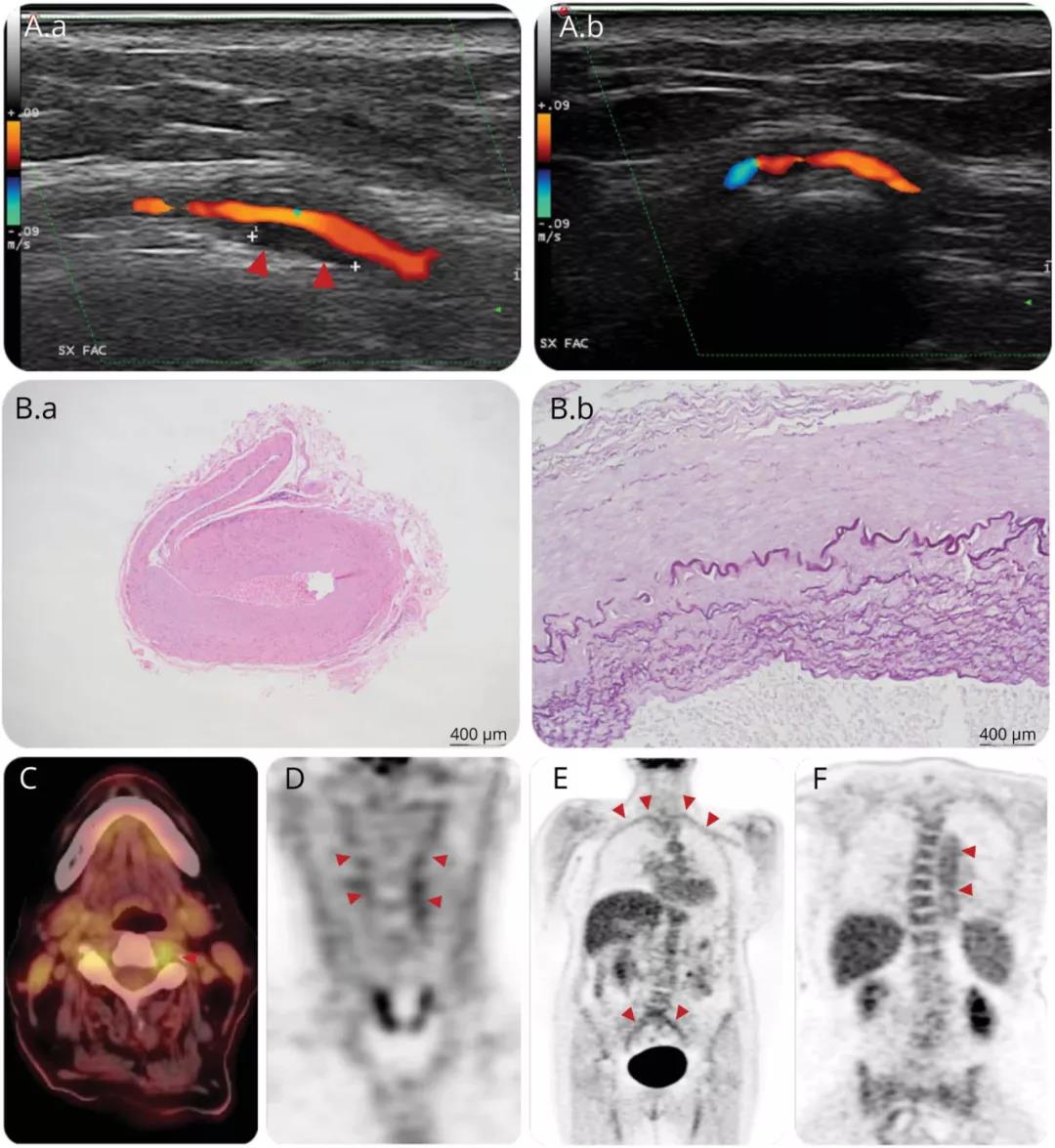
图2.面动脉多普勒超声显示低回声晕(A.a),治疗后消失(A.b)。治疗11天后的STAb显示内膜增厚和弹力层碎裂(B.a,B.b)。PET-CT显示椎动脉、锁骨下动脉、髂动脉和胸主动脉[18F]-FDG摄取。
尽管及时使用大剂量类固醇和托西利单抗治疗,这也使随后的颞动脉活检没有得到诊断信息(图2)。
原始出处:
Valentina Poretto, Silvio Piffer, Valeria Bignamini, et al. Progressive and Fatal Brainstem Stroke in Systemic Giant Cell Arteritis. Neurol Clin Pract. 2021 Dec;11(6):e965-e967. doi: 10.1212/CPJ.0000000000001083.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Neurol#
36
#动脉炎#
42
#巨细胞#
53
学习
35