EuroIntervention:CrossBoss导管可有效治疗支架内再狭窄
2014-05-28 佚名 dxy
冠脉慢性完全闭塞病变(CTO)事件是心脏介入治疗中复杂难治型病变,而且CTO的经皮冠状动脉介入治疗(PCI)成功率较低。另一方面,CTO事件多继发于支架内再狭窄(ISR)。因此,防治闭塞型ISR有十分重要的临床意义。针对上述问题,英国研究团队论证了一种新型导管——CrossBoss导管(器械来源为美国波士顿科学公司)在闭塞型ISR病变的治疗效果。研究者选取了英国地区30名患者,采用CrossBos
冠脉慢性完全闭塞病变(CTO)事件是心脏介入治疗中复杂难治型病变,而且CTO的经皮冠状动脉介入治疗(PCI)成功率较低。另一方面,CTO事件多继发于支架内再狭窄(ISR)。因此,防治闭塞型ISR有十分重要的临床意义。【原文下载】
针对上述问题,英国研究团队论证了一种新型导管——CrossBoss导管(器械来源为美国波士顿科学公司)在闭塞型ISR病变的治疗效果。
研究者选取了英国地区30名患者,采用CrossBoss导管作为CTO治疗首选治疗方式。入组患者共出现31例CTO,CTO持续时间中位数为24个月;患者CTO病变平均长度为39mm,既往PCI治疗手术失败比例为48%.手术成功率90%,在CrossBoss导管帮助下的直接成功率为81%.CrossBoss导管在多数CTO病例可以实施直接管腔贯通,而且治疗效果不理想的病例有明确的失败预测因素。
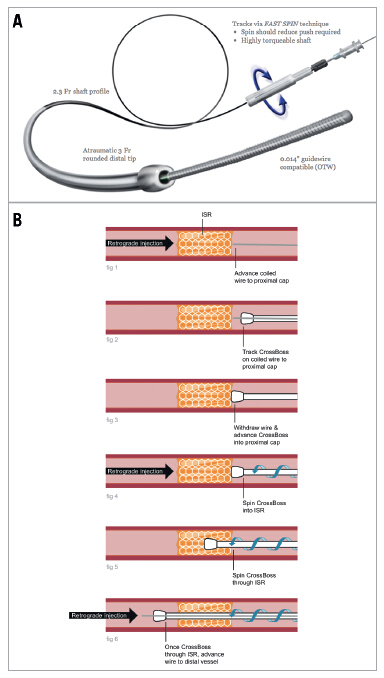
Figure 1. A) CrossBoss catheter (reproduced with permission of
Boston Scientific). B) Use of the CrossBoss catheter in occlusive
restenosis.
研究者认为CrossBoss导管治疗手术成功率高,放置导丝时间短且没有并发症,在治疗闭塞型ISR方面效果理想。
CrossBoss导管简介
该研究所使用的CrossBoss导管由美国波士顿科学公司提供,是一种6F外径OTW型导管(over-the-wire)。其冠脉导丝尖端为钝性无创性,直径3F(1mm),该设计允许术者在保证血管形态的基础上,手动快速旋转导管打通闭塞病变部位。
CrossBoss导管可以通过两种方式打通ISR闭塞,一种是直接经血管管腔,另一种是开通可控性内膜下通道。通过上述方式,CrossBoss导管可达到治疗CTO病变的目标。CrossBoss导管在难治性CTO病变的治疗效果在FAST-CTO研究中也得到了证实。
原始出处:
Wilson WM1, Walsh S, Hanratty C, Strange J, Hill J, Sapontis J, Spratt JC.A novel approach to the management of occlusive in-stent restenosis (ISR).EuroIntervention. 2014 Mar 20;9(11):1285-93. doi: 10.4244/EIJV9I11A218.【原文下载】
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#支架内再狭窄#
41
#CRO#
30
#ROS#
22
#再狭窄#
36
#有效治疗#
21