Front Oncol:局部晚期或转移性食管鳞状细胞癌患者在化疗基础上联合放疗可改善患者预后
2022-04-05 yd2015 网络
局部晚期或转移性食管鳞状细胞癌患者在化疗基础上联合放疗可改善患者预后。
近期,Frontiers in Oncology杂志上发表了一项来自广西医科大学附属肿瘤医院放疗科的研究成果,主要是评估在局部晚期或转移性食管鳞状细胞癌患者中,化疗联合放疗(CRT)对比单独化疗(CT)治疗的疗效比较。
我们回顾性评估了194例新诊断的晚期食管鳞癌患者,其接受CRT或CT治疗,包括97例局部晚期患者和97例远处转移患者。累积总生存期(OS)和无进展生存期(PFS)采用log-rank检验进行评估。倾向评分匹配被用来模拟随机分配。此外,我们对局部晚期和转移性疾病进行了亚组分析。
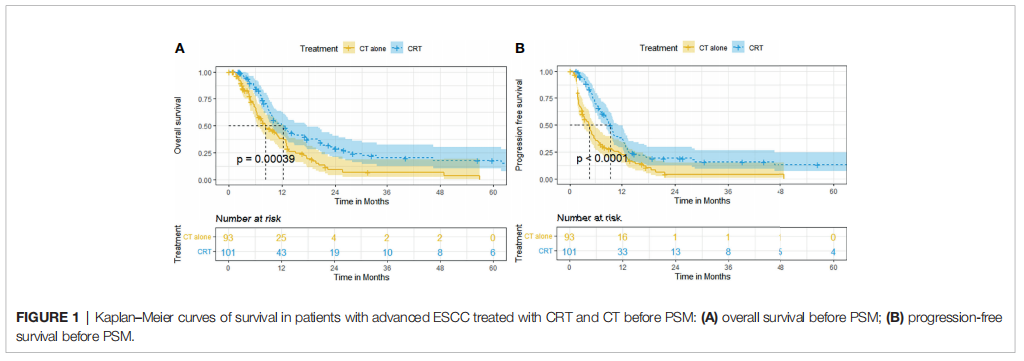
194例患者中,101例(52.1%)患者接受了CRT治疗,93例(47.9%)患者接受了CT治疗。倾向评分匹配后,两组中各有63例患者。
匹配之前,CRT组的中位OS,6、12、24和60个月的OS率要优于CT组(12.2个月(95% CI, 9.0 - 15.3), 84.1%, 50.8%, 29.0%, 17.9% vs 8.2个月(95% CI, 5.4 -11.1), 66.0%, 38.3%, 9.1%, 0%, p = 0.00039)。CRT组的中位PFS和6、12、24和60个月PFS率也优于CT组(9.4个月[95% CI, 8.0-10.8], 69.5%, 38.1%, 19.2%, 13.1% vs 4.7个月[95% CI, 3.5-5.9], 36.6%, 22.4%, 4.1%, 0%, p<0.0001)。
在调整所有基线因素后,CRT组和CT组在PFS和OS方面也有显著差异。CRT组的中位OS,6、12、24和60个月的OS率要优于CT组(12.5个月(95% CI, 7.1 - 18.0), 85.9%, 47.4%, 23.4%, 17.3% vs 7.6个月(95% CI, 5.4 - 9.8), 63.6%, 39.4%, 7.3%, 0%, p = 0.002)。CRT组的中位PFS和6、12、24和60个月PFS率也优于CT组(9.0个月(95% CI, 7.6 - 10.5), 70.9%, 36.5%, 19.7%, 12.9% vs 4.8个月(95% CI, 4.0 - 5.6), 39.1%, 22.7%, 3.8%, 3.8%, p = 0.0025)。
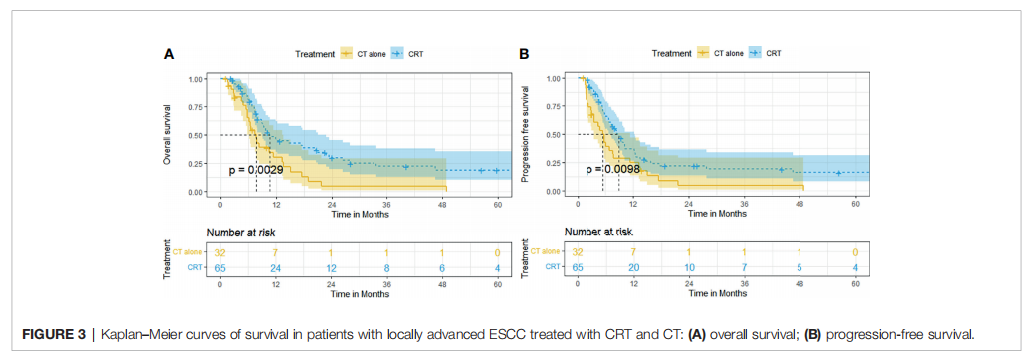
亚组分析时,在局部晚期ESCC患者中,CRT组的生存预后明显优于CT组。CRT组的中位OS,6、12、24和60个月的OS率要优于CT组(10.5个月(95% CI, 7.3 - 13.7), 79.8%, 46.6%, 29.8%, 18.9% vs 7.6个月(95% CI, 5.9 - 9.3), 65.4%, 30.3%, 4.3%, 0%, p = 0.0029)。CRT组的中位PFS和6、12、24和60个月PFS率也优于CT组(8.9个月(95% CI, 6.9 - 10.9), 65.7%, 37.3%, 22.0%, 16.0% vs 5.4个月(95% CI, 3.8 - 7.0), 42.8%, 25.0%, 4.5, 0%, p = 0.0098)。
在转移性ESCC患者中,CRT组的中位OS,6、12、24和60个月的OS率要优于CT组(12.9个月(95% CI, 10.2 - 15.7), 91.4%, 58.0%, 28.1%, 17.6%和9.3个月(95% CI, 5.7 - 13.0), 66.6%, 42.8%, 12.2%, 8.2%, p = 0.029)。CRT组的中位PFS和6、12、24和60个月PFS率也优于CT组(9.9个月(95% CI, 7.9 - 11.9), 76.5%, 39.9%, 14.7%, 9.8%和4.0个月(95% CI, 2.4 - 5.7), 33.4%, 20.8%, 3.7%, 3.7%, p = 0.0032)。

在匹配前队列多因素分析,放疗的加入,白蛋白水平,绝对中性粒细胞计数,和化疗周期数是OS(p = 0.041, p = 0.000, p = 0.001, p = 0.002)和PFS (p = 0.007, p = 0.02, p = 0.02, p = 0.000)的独立预后因素。同时,N分期和转移部位数是PFS (p = 0.015和p = 0.007)的独立预后因素。
综上,研究表明,局部晚期或转移性食管鳞状细胞癌患者在化疗基础上联合放疗可改善患者预后。
原始出处:
Li L-Q, Fu Q-G, Zhao W-D, Wang Y-D, Meng W-W and Su T-S (2022) Chemoradiotherapy Versus Chemotherapy Alone for Advanced Esophageal Squamous Cell Carcinoma: The Role of Definitive Radiotherapy for Primary Tumor in the Metastatic Setting. Front. Oncol. 12:824206. doi: 10.3389/fonc.2022.824206
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Oncol#
31
#局部晚期#
36
#患者预后#
30
#细胞癌#
28
#联合放疗#
40
#食管鳞状细胞癌#
58
#转移性#
30
#局部#
25
#食管#
28