ESMO 2022:替雷利珠单抗作为不可切除HCC一线治疗显示出非劣效于索拉非尼的OS获益(RATIONALE 301研究)
2022-09-12 MedSci原创 MedSci原创
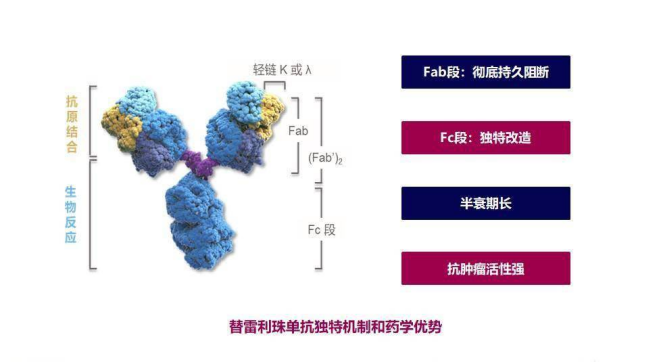
替雷利珠单抗是一种人源化的PD-1抗体。替雷利珠单抗的Fc段经过基因工程的改构,所以,当它在跟巨噬细胞的Fcγ受体结合的时候,能够消除抗体依赖的细胞介导的吞噬作用(ADCP效应),从而降低
替雷利珠单抗是一种人源化的PD-1抗体。替雷利珠单抗的Fc段经过基因工程的改构,所以,当它在跟巨噬细胞的Fcγ受体结合的时候,能够消除抗体依赖的细胞介导的吞噬作用(ADCP效应),从而降低T细胞的耗竭,加强细胞免疫的功能,这是其跟其它抗体比较的一个特点。另外,替雷利珠单抗的Fab段跟PD-1分子结合的亲和力非常强,解离速度却缓慢,能够保持对PD-1的高亲和力和低解离速率,彻底激活身体里杀伤肿瘤的作用。
RATIONALE -301是一项全球性的III期随机、开放标签、多中心研究,评估与索拉非尼相比,替雷利珠单抗作为成人不可切除HCC患者的一线治疗的疗效和安全性。该研究的主要终点是比较两个治疗组之间的OS。根据此次公布的数据来看,替雷利珠单抗单药治疗晚期肝癌的OS并不劣效于索拉非尼。此外,本研究还有一个关键的次要终点——ORR,暂未披露是否达到预期结果。
根据在2022年ESMO大会上公布的III期RATIONALE-301试验(NCT03412773)的最终分析数据,替雷利珠单抗单药治疗提供了具有临床意义的总生存期(OS)获益,非劣效于索拉非尼(多吉美),并且在不可切除的肝细胞癌(HCC)患者的一线治疗中表现出更低的毒性特征。
大会摘要显示,在随访时间至少33个月时,替雷利珠单抗组的中位OS为15.9个月(95%CI,13.2-19.7个月),与对照组(索拉非尼)相比(14.1个月,95%CI,12.6-17.4个月)达到非劣效性标准(HR:0.85;95.003%CI,0.712-1.019,P=0.0398)。替雷利珠单抗组的客观缓解率为14.3%,优于活性对照组(5.4%)。替雷利珠单抗组的中位缓解持续时间为36.1个月,对照组这一数值为11.0个月。
根据主要研究者、日本近畿大学医学部附属医院Masatoshi Kudo教授在大会上介绍的最终分析结果,在所有亚组中也观察到这种OS获益。
OS支持替雷利珠单抗的关键亚组包括年龄≥65岁的患者(HR0.76;95%CI,0.57-1.02)、无微血管浸润和/或肝外转移的患者(HR0.78;95%CI,0.56-1.07)、丙型肝炎感染患者(HR0.64;95%CI,0.38-1.08)和女性患者(HR0.62;95%CI,0.39-0.99)。
“目前还没有单药检查点抑制剂在这种情况下被批准,”Kudo在解释这项研究的背景时解释道, “替雷利珠单抗是一种单克隆抗体,与PD-1具有杂交结合亲和力,经过专门设计,可使巨噬细胞上的FCyγ受体结合最小化。在既往接受过治疗的晚期HCC患者中,替雷利珠单抗单药治疗逐渐表现出持久的缓解,并且通常耐受性良好。”
本研究将674例患者以1:1的比例随机分配至200mg替雷利珠单抗静脉给药每3周一次组(n=342)或400mg索拉非尼口服给药每日两次组(n=332)。符合入组条件的患者须患有组织学证实的HCC、未接受过全身治疗、Child-Pugh A级、ECOG体能状态评分为1分,且无累及门静脉主干或下腔静脉的癌栓。患者继续接受治疗,直至疾病进展或出现不可耐受的毒性。
研究主要包括亚洲患者(不包括日本),替雷利珠单抗组为62.9%(n=215),索拉非尼组为63.3%(n=210)。接受研究药物或对照药物治疗的日本患者分别占11.1%和11.7%,其他地区的患者分别为26.0%和25.0%。替雷利珠单抗组和索拉非尼组患者的中位年龄相当,分别为62岁(25.0-86.0)和60岁(23.0-86.0)。此外,两组中超过80%的患者为男性,超过75%的患者在入组时为Barcelona-Clinic肝癌C期,超过70%的患者ChildPugh评分为5。大多数患者还患有乙型肝炎,替雷利珠单抗组为59.4%,对照组为62.0%。
在评估这些患者是否持续缓解时,替雷利珠单抗组的ORR高于索拉非尼组,分别为14.3%(95%CI,10.8%-18.5%)和5.4%(95%CI,3.2%-8.4%)。此外,替雷利珠单抗组有10例完全缓解,索拉非尼组有1例患者完全缓解。然而,索拉非尼组有139例患者病情稳定,而研究组有94例,而研究组有169例患者病情进展,索拉非尼组有121例。
替雷利珠单抗治疗有缓解的患者(n=49)的中位缓解持续时间,也长于索拉非尼治组(n=18),分别为36.1个月和11个月。在这些患者中,71.4%的患者接受替雷利珠单抗治疗后持续缓解,40.0%的患者接受索拉非尼治疗后持续缓解。然而,索拉非尼组的中位无进展生存期长于替雷利珠单抗组,分别为3.6个月(95%CI,2.2-4.1)和2.2个月(95%CI,2.1-3.5)(HR,1.11;95%CI,0.92-1.33)。
替雷利珠单抗组治疗中出现的不良反应(TEAE)和≥3级治疗相关AE的发生率较低,分别为48.2%和22.2%,而索拉非尼组分别为65.4%和53.4%。与索拉非尼相比,替雷利珠单抗的停药率和剂量调整率也较低,分别为10.9%和31.1%,而索拉非尼分别为18.5%和64.8%。然而,替雷利珠单抗组和索拉非尼组导致死亡的TEAE相当,分别为4.4%和5.2%。
替雷利珠单抗组的≥3级天门冬氨酸氨基转移酶和/或丙氨酸氨基转移酶升高、血胆红素升高、血小板计数降低和腹泻的发生率低于50%,相比之下索拉非尼组的上述发生率较高。Kudo指出,这在高血压组中尤其如此,只有接受索拉非尼治疗的患者出现3级或3级以上的掌跖红肿疼痛。
“总之,与索拉非尼相比,替雷利珠单抗单药治疗在该患者群体中,表现出具有临床意义的抗肿瘤获益,且安全性特征良好、可控,”Kudo说。“我们希望在未来的医学会议上对这些数据提供进一步的见解。”
参考资料:
BeiGene announces positive global phase 3 trial results fro PD-1 inhibitor tislelizumab in first-line unresectable hepatocellular carcinoma. News release. BeiGene. August 9, 2022. Accessed August 9, 2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#非劣效#
40
#SMO#
46
#ratio#
40
#HCC#
62
#ESMO#
30