DES术后双联抗血小板治疗:何时停药?
2012-05-26 李毅 沈阳军区总医院
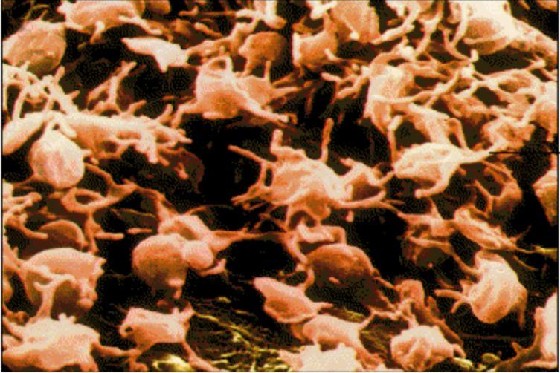
药物洗脱支架(DES)的广泛应用显著降低了冠状动脉介入治疗(PCI)术后再狭窄率,但是,2006年前后发表的一系列临床研究和病理学研究均提示,第一代涂层不可降解DES的迟发支架血栓风险明显高于裸金属支架(BMS),因此国内外现行的指南均推荐在DES术后接受双联抗血小板治疗(DAPT)至少1年,除非病人存在出血高危因素。但长期DAPT是一柄双刃剑,在降低血栓风险的同时,不仅导致医疗费用的显著增高,而
药物洗脱支架(DES)的广泛应用显著降低了冠状动脉介入治疗(PCI)术后再狭窄率,但是,2006年前后发表的一系列临床研究和病理学研究均提示,第一代涂层不可降解DES的迟发支架血栓风险明显高于裸金属支架(BMS),因此国内外现行的指南均推荐在DES术后接受双联抗血小板治疗(DAPT)至少1年,除非病人存在出血高危因素。但长期DAPT是一柄双刃剑,在降低血栓风险的同时,不仅导致医疗费用的显著增高,而且可使患者出血风险明显增高。另一方面,随着新型DES的问世、手术技术和策略的改进、血管内影像评价技术的不断普及以及围术期二级预防治疗的日渐规范,目前文献报道DES术后迟发支架内血栓的年发生率仅0.1%~0.5%,针对这样一个发生率进行超过1年的长期DAPT是否具有效价比还值得商榷。迄今为止,DES术后DAPT如何达到疗效与成本的最佳平衡点仍是一个悬而未决的问题。 BASKET-LATE研究之后,又有许多临床研究支持DES术后进行超过1年的长期DAPT。2009年发表的TYCOON研究前瞻性入选了447例DES术后患者,其中2003年入选的173例患者接受12个月DAPT,2004年入选的274
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#双联抗血小板#
31
#停药#
26
#双联抗血小板治疗#
34
#DES#
33
#DES#
32