Angew. Chem.:德国研究人员发现芋螺毒素可以用于癌症疼痛治疗
2012-05-19 政策研究与驻外指导处 政策研究与驻外指导处
近日,德国波恩大学和耶拿大学研究人员利用核磁共振成像扫描技术确定了芋螺毒素的混合成分构成。研究人员发现名为μ-PIIIA的不同折叠类型的多肽毒素虽然作用相似,但它们之间也有存在很大区别。该项研究发现对于开发新型止痛药物具有重要意义,芋螺毒素有望应用在癌症患者止痛治疗领域。目前,其相关研究成果已经在2012年《应用化学杂志》上刊登。 芋螺是一种生活在海底依靠毒素捕猎的动物,其少量毒素就会破坏神经

近日,德国波恩大学和耶拿大学研究人员利用核磁共振成像扫描技术确定了芋螺毒素的混合成分构成。研究人员发现名为µ-PIIIA的不同折叠类型的多肽毒素虽然作用相似,但它们之间也有存在很大区别。该项研究发现对于开发新型止痛药物具有重要意义,芋螺毒素有望应用在癌症患者止痛治疗领域。目前,其相关研究成果已经在2012年《应用化学杂志》上刊登。
芋螺是一种生活在海底依靠毒素捕猎的动物,其少量毒素就会破坏神经系统的信号传输。毒性最大的芋螺足以使人在受到攻击后1根香烟时间内致命。与此同时,芋螺毒素也可以用于治疗疼痛。研究人员在实验鼠体内进行的研究已表明,芋螺毒素可以有效缓解哺乳动物的疼痛症状。为此,研究人员认为芋螺毒素可用于普通止疼药已经无效的癌症疼痛患者和慢性疼痛患者,而且由于芋螺毒素在人体内代谢速度很快,将不会使患者形成药物依赖性。
在未来,芋螺毒素实现临床应用所面临的障碍是提炼出形式稳定的芋螺毒素。为此,相关研究人员正在联合开展芋螺µ-PIIIA毒素稳定性研究。

doi:10.1002/anie.201107011
PMC:
PMID:
Structurally Diverse μ-Conotoxin PIIIA Isomers Block Sodium Channel NaV1.4
lesia A. Tietze1, Dr. Daniel Tietze2, Dr. Oliver Ohlenschläger3, Dr. Enrico Leipold4, Florian Ullrich4, Toni Kühl1,4, André Mischo3, Prof. Dr. Gerd Buntkowsky2, Dr. Matthias Görlach3, Prof. Dr. Stefan H. Heinemann4, Prof. Dr. Diana Imhof
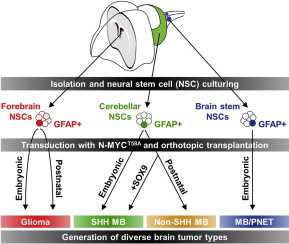
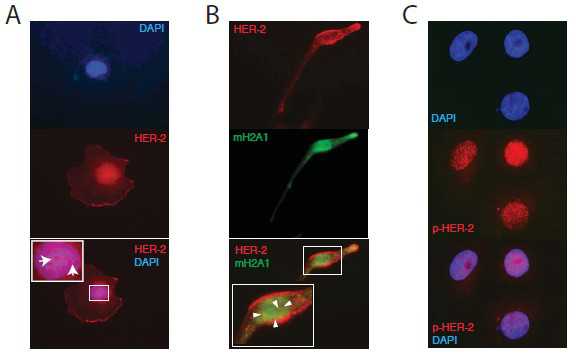
Three chemically synthesized μ-conotoxin PIIIA isomers (see picture), which contain different disulfide connectivity, block the skeletal muscle voltage-gated sodium channel NaV1.4 with similar, yet distinguishable potency. Hence, bioactivity of this μ-conotoxin is not strictly coupled to its native fold. Future development of conotoxin-derived analgesics may benefit from such a widened structural repertoire.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#疼痛治疗#
34
#研究人员#
40
#Angew#
28
#德国#
27
#癌症疼痛#
36