Thorac Cancer:伴有罕见突变的晚期或转移性NSCLC患者的真实世界数据
2021-12-11 yd2015 MedSci原创
研究表明,一线铂类化疗对伴有罕见突变的非鳞状NSCLC患者具有持久临床疗效。
肺腺癌是非小细胞肺癌(NSCLC)常见的类型。EGFR和ALK突变是常见的突变类型。针对两者的靶向治疗明显改善晚期患者的预后。但是,对于伴有罕见突变(除外EGFR和ALK突变)的NSCLC患者,目前在真实世界中数据仍比较有限。因此,有韩国学者开展了回顾性研究,评估伴有罕见突变的非鳞状NSCLC的疗效和临床预后。相关结果发表在Thoracic Cancer杂志上。
研究回顾性纳入韩国9家三级医院2015年1月至2020年9月期间,年龄>20岁的晚期或转移性非鳞状NSCLC患者,其证实伴有罕见突变(BRAF、ROS1、MET、RET、HER2、FGFR和NTRK)。
研究纳入伴有罕见突变的118例晚期或转移性非鳞状NSCLC患者。中位年龄61岁,男性占44.1%,39%的患者有吸烟史。17例(14.4%)患者初始诊断伴有脑转移。在118例患者中,46例(39%)ROS1突变,27例(22.9%)RET突变,14例(11.9%)MET突变,14例(11.9%)ERBB2突变,10例(8.5%)BRAF突变,5例(4.2%)FGFR突变,2例(1.7%)NTRK突变。NGS诊断81例(68.6%),RT- PCR诊断37例(37%)。107例患者接受姑息性化疗,88例患者接受铂类化疗作为一线化疗。其中58例患者接受铂联合培美曲塞治疗。13例患者接受克唑替尼一线化疗,均为ROS 1突变患者。
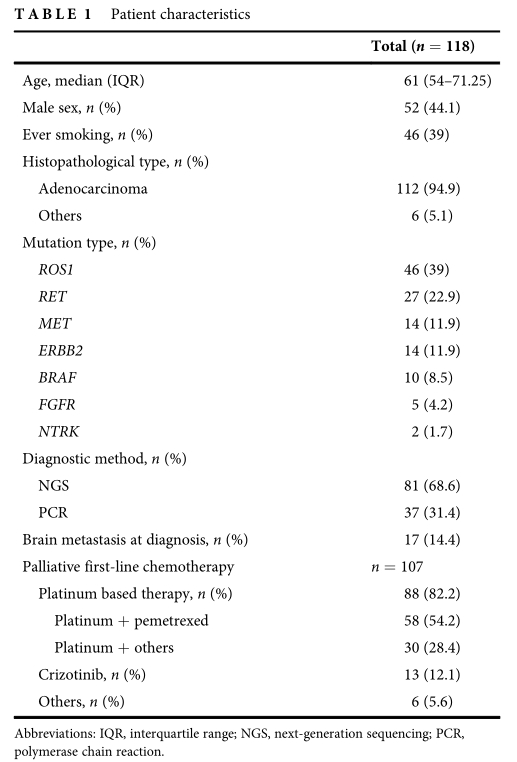
临床特征
ROS1、RET、MET、ERBB2和BRAF突变患者接受姑息性一线铂类化疗的中位无进展生存期(PFS)和总生存期(OS)类似。中位随访时间为15.8个月(IQR 7.5-27.8)。他们的中位PFS和OS分别为9.6个月(95%CI: 7.7-11.5)和36.9个月(95% CI: 11.3-62.6)。BRAF、ERBB2、MET、RET、ROS1突变患者的中位PFS分别为10.9个月(95% CI: 1.3-20.5)、5.3个月(95% CI: 3.0-7.5)、7.2个月(95% CI: 3.6-10.9)、11.4个月(95% CI: 9.2-13.6)和10.0个月(95% CI: 3.7-16.4) (p = 0.041)。
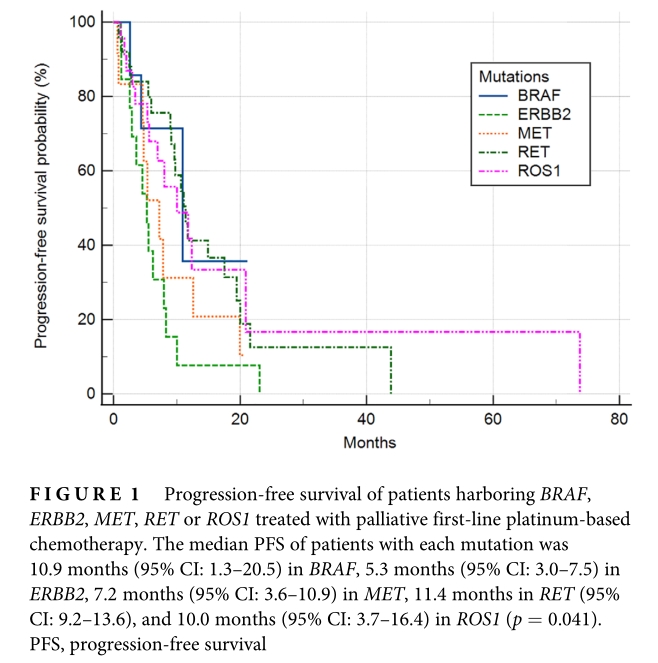
不同突变患者的PFS
BRAF、ERBB2、MET和RET突变患者的中位OS分别为14.1个月(95% CI: 10.1-14.1)、34.5个月(95% CI: 13.2-36.9)、22.7个月(95% CI: 1.7-24.0)和29.8个月(95% CI: 28.9-61.3) (p = 0.006)。而ROS1突变患者的中位OS尚未达到。
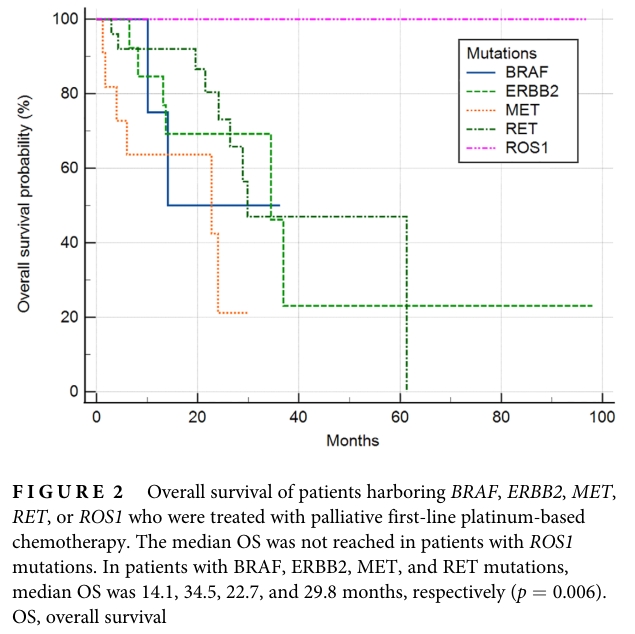
不同突变患者的OS
接受一线铂类化疗或克唑替尼的ROS1患者的中位PFS分别为10.0个月(95% CI: 3.7-16.4)和未达到(p = 0.399)。
接收一线铂类化疗患者的总客观缓解率(ORR)为37.0% (95% CI: 26.6-48.5),疾病控制率(DCR)为77.8% (95% CI: 67.2-86.3)。BRAF突变患者ORR和DCR分别为0% (n = 0/8)和75% (n = 6/8);ERBB2突变患者ORR和DCR分别为53.8% (n = 7/13) 和76.9% (n = 10/13);MET突变患者ORR和DCR分别为25% (n = 3/12)和66.7% (n = 8/12);RET突变患者ORR和DCR分别为52% (n = 13/25)和80% (n = 20/25);ROS1突变患者ORR和DCR分别为30.4% (n = 7/23)和82.6% (n = 19/23)。
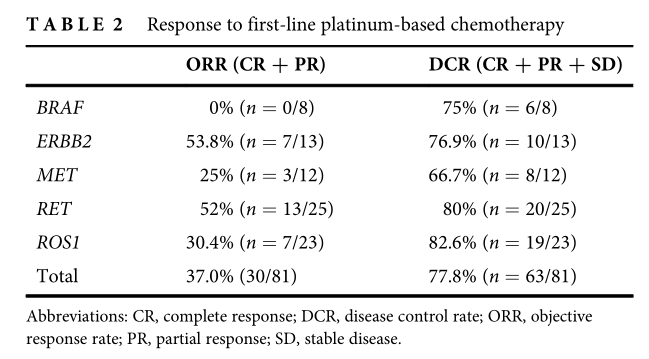
不同突变患者的ORR和DCR
综上,研究表明,一线铂类化疗对伴有罕见突变的非鳞状NSCLC患者具有持久临床疗效。
原始出处:
Lee SY, Kim YC, Lee KY, Lee SY, Lee SY, Lee MK, Lee JE, Jang SH, Jang TW, Choi CM. Multicenter real-world data of patients harboring rare mutations other than EGFR or ALK in advanced or metastatic non-small cell lung cancer. Thorac Cancer. 2021 Dec 8. doi: 10.1111/1759-7714.14266. Epub ahead of print. PMID: 34881519.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#转移性NSCLC#
35
#THORAC#
42
#SCLC患者#
38
学习了
58
#真实世界#
33
#转移性#
29
#NSCLC患者#
33
#罕见#
36