Scientific Reports:一种新型、智能、肿瘤靶向的磁共振造影剂
2013-01-14 中国科学技术大学 Scientific Reports
1月3日,国际学术期刊Scientific Reports在线发表了中国科学技术大学梁高林教授课题组和中山大学肿瘤防治中心李立课题组的合作研究成果,文章标题为Controlled intracellular self-assembly of gadolinium nanoparticles as smart molecular MR contrast agents。该文章报导了一种新型、智能、肿瘤
1月3日,国际学术期刊Scientific Reports在线发表了中国科学技术大学梁高林教授课题组和中山大学肿瘤防治中心李立课题组的合作研究成果,文章标题为Controlled intracellular self-assembly of gadolinium nanoparticles as smart molecular MR contrast agents。该文章报导了一种新型、智能、肿瘤靶向的磁共振造影剂的研制,并在肿瘤模型小鼠上验证了其优异的肿瘤靶向成像效果。
核磁共振显像(MRI)是目前临床上普遍使用的一种功能影像方法,此技术对检测组织坏死、局部缺血及各种病变具有独特的优势。因其具有较高的分辨率,在临床医学上对疾病早期诊断也显示出巨大的应用前景。目前临床使用的磁共振造影剂大都为小分子,采用纳米材料作为载体用来装载造影剂以提高生物组织局部的造影剂浓度已经成为研究热点。然而,基于纳米材料的这类造影剂除了要克服制备方面的技术难度外,还要面对低摄取和靶向难等问题。
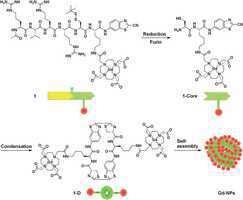
继利用梁高林博士发展出的一个独特的缩合反应平台成功研制出第一代磁共振造影剂后,该课题组此次与中山大学肿瘤中心和南京大学金陵医院合作,成功研制出第二代肿瘤靶向智能磁共振造影剂。该技术把两个用于缩合反应的官能团设计到一个含Gd的磁性小分子上,在肿瘤细胞内的还原剂和高表达的蛋白酶作用下,小分子化合物发生缩合反应生成多聚体,两亲性的多聚体在肿瘤细胞内自组装成磁性纳米粒子,从而产生大大高于小分子单体的MRI信号。
论文第一作者为中国科大博士生曹春艳和中山大学博士生沈莹莹。该项目研究得到国家自然科学基金,安徽省杰出青年科学基金和中国科大重要方向项目培育基金的资助。(生物谷Bioon.com)

doi:10.1038/srep01024
PMC:
PMID:
Chun-Yan Cao,1 Ying-Ying Shen,2 Jian-Dong Wang,3 Li Li2 & Gao-Lin Liang1
Herein we developed a new “smart” Gd-based MR contrast agent (i.e., 1) which is susceptive to furin, a protease overexpressed in tumor. Under the action of furin, 1 condenses to form dimers (1-Ds) and the latter self-assemble into gadolinium nanparticles (Gd-NPs). Relaxivity of 1-D is more than 2 folds of those of 1 and magnevist at 1.5 T, and 1.4 folds of that of 1 at 3 T. Intracellular condensation of 1 in furin-overexpressed MDA-MB-468 cells was proven with direct two-photon laser microscopy (TPLM) fluorescence imaging of the cells incubated with the europium analog of 1 (i.e., 2). Intracellular Gd-NPs of 1 were uncovered and characterized for the first time. MRI of MDA-MB-468 tumors showed that 1 has enhanced MR contrast within the tumors than that of its scrambled control 1-Scr.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#肿瘤靶向#
17
#磁共振#
32
#SCIE#
22
#造影#
25