Br J Surg:甲状腺乳头状癌术中未预防性清扫颈淋巴结的结局分析
2016-02-17 Mechront 译 MedSci原创
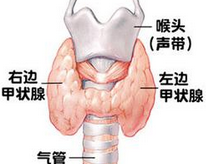
甲状腺乳头状癌(PTC)的治疗过程中是否需要预防性清扫颈淋巴结(CND)仍存在争议。研究者纳入了1986-2010年间没有行CND的所有PTC患者。在术前和围手术期,对所有患者的颈部进行仔细的临床评估,是否存在任何可疑需切除的淋巴结组织。该队列中包含了淋巴结切除的患者,但是没有一例患者是经过了正式的颈部解剖的淋巴结清扫。通过Kaplan-Meier方法计算患者的无复发生存率(RFS)和颈部中央RF
甲状腺乳头状癌(PTC)的治疗过程中是否需要预防性清扫颈淋巴结(CND)仍存在争议。
研究者纳入了1986-2010年间没有行CND的所有PTC患者。在术前和围手术期,对所有患者的颈部进行仔细的临床评估,判断是否存在任何可疑需切除的淋巴结组织。该队列中包含了淋巴结切除的患者,但是没有一例患者经过了正式的颈部解剖的淋巴结清扫。通过Kaplan-Meier方法计算患者的无复发生存率(RFS)和颈部中央RFS以及基本特异性生存率(DSS)。
该研究涉及的1798名患者中有397人(22.1%)为男性,有1088人(60.5%)年龄≥45岁,有539人(30.0%)伴有pT3或pT4疾病。有742人(41.3%)接受了放射性碘的辅助治疗。中位数随访46个月,5年DSS为100%,5年RFS为96.6%,5年颈部中央RFS为99.1%。
研究结果表明,在术前和术中对PTC患者颈部中央进行详细的观察,以确认是否有颈部中央淋巴结转移是安全的。
原始出处:
Nixon IJ, Wang LY,et al.Outcomes for patients with papillary thyroid cancer who do not undergo prophylactic central neck dissection.Br J Surg. 2016 Feb;103(3):218-25. doi: 10.1002/bjs.10036.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#乳头状#
24
#预防性#
27
这个研究要好好看看
98
#淋巴结#
29
#甲状腺乳头状癌#
29