TCT2018:里程碑式研究:介入治疗心衰合并二尖瓣反流降低38%死亡率
2018-09-26 xujing 中国循环杂志
TCT大会主席Gregg W. Stone教授公布了COAPT研究结果,首次证实了二尖瓣钳夹术(MitraClip)治疗继发于左心功能衰竭的二尖瓣严重反流的安全性和有效性,MitraClip能使这类患者的死亡率降低38%。
TCT大会主席Gregg W. Stone教授公布了COAPT研究结果,首次证实了二尖瓣钳夹术(MitraClip)治疗继发于左心功能衰竭的二尖瓣严重反流的安全性和有效性,MitraClip能使这类患者的死亡率降低38%。
该研究结果同步刊登在新英格兰医学杂志上。
MitraClip是首个被证实是可以改善继发于左心功能衰竭的二尖瓣严重反流患者预后的治疗方法。
COAPT研究共计纳入610例心力衰竭合并中-重度或重度二尖瓣反流患者,在应用最大耐受剂量药物治疗后仍有症状的患者。
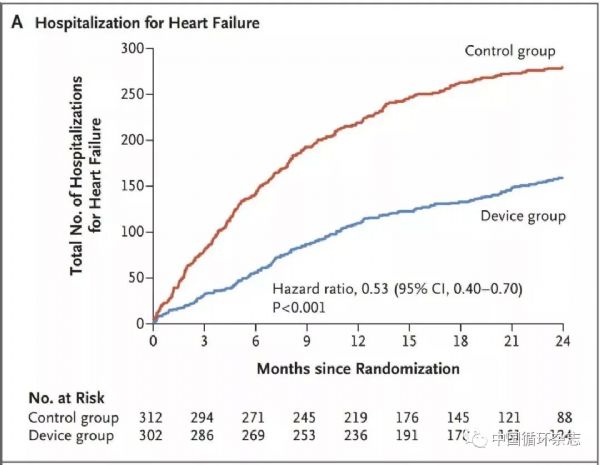
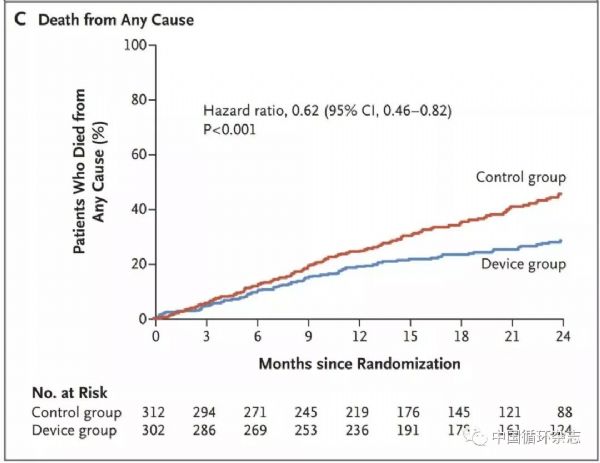
312例患者给予最大耐受剂量的优化药物治疗,302例在优化药物治疗的基础上联合使用MitraClip。随访2年。主要终点包括有效性终点(两年内因心衰再入院率)及安全性终点(12个月内器械相关并发症)。
结果显示,药物治疗患者的再住院率为67.9%,MitraClip治疗患者为35.8%,相对下降了47%。
药物治疗患者的2年死亡率为46.1%,MitraClip治疗患者为29.1%,死亡率相对下降38%。
此外,MitraClip治疗患者的无器械相关并发症的12个月生存率为96.6%。
原始出处:
Stone GW, et al. Transcatheter mitral-valve repair in patients with heart failure. N Engl J Med, 2018. DOI:10.1056/NEJMoa1806640.
小提示:本篇资讯需要登录阅读,点击跳转登录
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#里程碑式研究#
29
#里程碑#
33
#TCT#
30
#二尖瓣#
35
#反流#
28