J Natl Cancer I:不同剂量HPV16/18疫苗接种7年后效果如何?
2017-10-31 吴星 环球医学
2018年2月,发表在《J Natl Cancer Inst》的一项研究调查了接受不同剂量HPV16/18疫苗的女性在接种疫苗后7年保护作用的持续情况及抗体水平。结果显示,在平均随访7年时间中,研究者观察到不同剂量组相似的HPV16/18低感染率,以及抗体水平的略微降低。
2018年2月,发表在《J Natl Cancer Inst》的一项研究调查了接受不同剂量HPV16/18疫苗的女性在接种疫苗后7年保护作用的持续情况及抗体水平。结果显示,在平均随访7年时间中,研究者观察到不同剂量组相似的HPV16/18低感染率,以及抗体水平的略微降低。
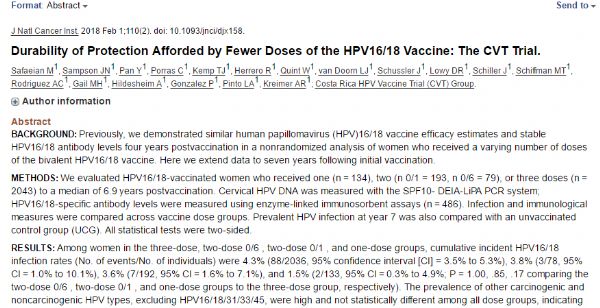
背景:此前,研究者在一项考察女性接受不同剂量二价人乳头状瘤病毒(HPV)疫苗的非随机分析中证实了HPV 16/18疫苗的有效性相似,且接种疫苗后4年的抗体水平稳定。在此,研究者将初始疫苗接种的数据扩展至7年。
方法:研究者评价了直至接种后中位6.9年,接种1剂(134例)、2剂(0/1,193例;0/6,79例)或3剂(2043例)HPV16/18疫苗的女性。使用SPF10- DEIA-LiPA PCR系统,测量子宫HPV DNA;使用联免疫吸附剂测定测量特定HPV16/18抗体的水平(486例)。比较不同剂量组的感染和免疫指标。在第7年,比较接种组与非接种对照组(UCG)之间的HPV病毒感染情况。所有统计学检测均为双边。
结果:在3剂组、2剂0/6组、2剂0/1组和1剂组中,HPV16/18累积感染率(事件数量/个体数量)分别为4.3%(88/2036,95%置信区间[CI] = 3.5%~5.3%)、3.8%(3/78,95% CI?=?1.0%~10.1%)、3.6%(7/192,95% CI?=?1.6%~7.1%)和1.5%(2/133,95% CI?=?0.3%~4.9%;2剂0/6组、2剂0/1组和1剂组与3剂组相比P 分别= 1.00、0.85和0.17)。排除HPV16/18/31/33/45,其他癌症及非致癌HPV型患病率高,且在所有组中没有显着性差异,表明,1剂接种和2剂接种组的低HPV16/18感染风险与缺少疫苗暴露无关。第7年,所有剂量组100%的受试者保持HPV16和HPV18血清反应阳性。在3剂组:–10.8%(95% CI =–25.3%~6.6%)、2剂(0/6个月)组:–17.3%(95% CI =–39.3%~12.8%)、2剂(0/1个月)组:–6.9%(95% CI =–22.1%~11.2%)和1剂组:–5.5%(95% CI =–29.7%~27.0%)的女性中观察到4至7年HPV16抗体水平的几何平均数有非统计学意义的显着降低。HPV18的结果相似。
结论:在平均随访7年时间中,研究者观察到不同剂量组相似的HPV16/18低感染率,且抗体水平的略微降低。
原始出处:
Safaeian M,et al.Durability of Protection Afforded by Fewer Doses of the HPV16/18 Vaccine: The CVT Trial.J Natl Cancer Inst. 2018 Feb 1;110(2).
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言







#ATL#
20
#Nat#
22
#疫苗接种#
22