JNCI:PET检查能改善癌症患者预后吗?
2016-03-05 Mechront 译 MedSci原创
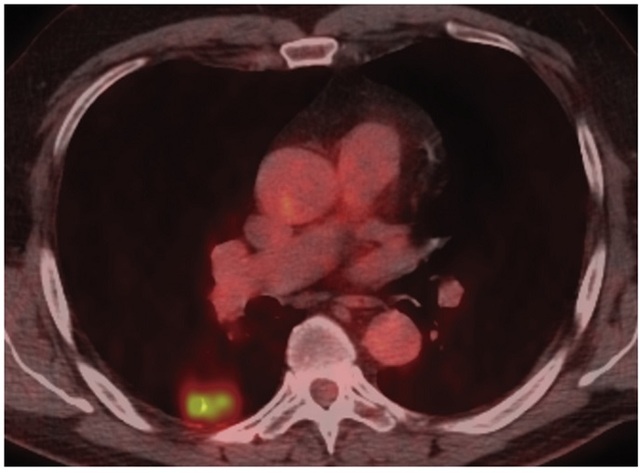
癌症患者常通过正电子发射断层扫描(PET)扫描进行肿瘤分期和再分期,以及对疗效进行监测。此外,通过PET还可以发现无症状的复发者,不过PET检查能否改善预后尚不明确。因此研究者进行了一项研究,评估PET检查对肺癌和食管癌患者预后的影响。
背景:癌症患者常通过正电子发射断层扫描(PET)扫描进行肿瘤分期和再分期,以及对疗效进行监测。此外,通过PET还可以发现无症状的复发者,不过PET检查能否改善预后尚不明确。因此研究者进行了一项研究,评估PET检查对肺癌和食管癌患者预后的影响。
方法:通过SEER和医疗相关数据库,研究者纳入了2005-2009年间的97152名肺癌和4446名食管癌患者。使用患者和肿瘤特征计算校正风险后的2年总生存率。研究者还调查了PET的使用率(以人/年为单位),不包括分期扫描和CT扫描后的随访。此外,研究者还探究了不同医院PET使用情况,以校正2年总生存率。
结果:不同医院的肺癌和食管癌患者PEF使用率差异很大,使用率最低和最高的医院相比较:肺癌 0.05/人年 (SD = 0.04) vs 0.70/人年 (SD = 0.44);食管癌 0.12/人年 (SD = 0.06) vs 0.97/人年 (SD = 0.29)。PET使用率最低和最高的医院比较校正后2年生存率:肺癌 29.0% (SD = 12.1%) vs 28.8% (SD = 7.2%)(P = .66);食管癌 28.4%
(SD = 7.2%) vs 30.3% (SD = 5.9%)(P = .55)。
结论:尽管在检测肿瘤复发上,PET的使用情况存在差异,但是对2年生存率并没有改善。此外,对肿瘤复发的检测上,可能存在PET的过度使用。
原始出处:
Healy MA, Yin H,et al.Use of Positron Emission Tomography to Detect Recurrence and
Associations With Survival in Patients With Lung and Esophageal Cancers.J Natl
Cancer Inst. 2016 Feb 22;108(7). pii: djv429. doi: 10.1093/jnci/djv429. Print
2016 Jul.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#PET检查#
44
#PE#
28
#NCI#
24
#患者预后#
33
过度使用?考虑复发了再做PET漏掉的多不...
132
对肿瘤复发的检测上,可能存在PET的过度使用。?
92
#癌症患者#
28
#PET#
26