Clin Cancer Res:新型PD-L1抗体TQB2450联合安罗替尼治疗局部晚期/转移性软组织肉瘤
2022-06-15 MedSci原创 MedSci原创
TQB2450联合安罗替尼在腺泡状软组织肉瘤中的疗效可期。
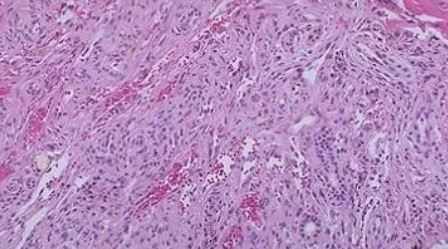
软组织肉瘤(STS)是一种罕见的异质性恶性肿瘤,起源于间质结缔组织。目前已发现了50多种不同组织亚型的STS,约占所有成人恶性肿瘤的1%和儿童恶性肿瘤的15%。
手术是大部分STS患者的主要标准治疗方法。但是,相当一部分患者确诊时已是局部晚期或已发生转移,错失手术机会,只能进行系统治疗。基于蒽环类药物的化疗是标准的一线系统治疗。对于一线治疗失败的患者,抗血管生成疗法是一种重要的治疗选择。抗PD-L1抗体也在STS中显示出了抗肿瘤活性。但PD-L1单克隆抗体和抗血管生成药物联用在STS中的潜力尚不明确。
TQB2450是一种PD-L1的新型人源单克隆抗体,与安罗替尼联用已在多种肿瘤中展现出可喜的抗肿瘤活性。
TQB2450-Ib-02研究是一项在我国的两家医院联合开展的单中心2期试验,旨在探究TQB2450联合安罗替尼用于局部晚期或转移性STS(LA/M STS)患者的疗效和安全性。
招募了既往至少对一种化疗不敏感的患者,予以安罗替尼(12 mg,1/日)口服(第1天-第14天/21天),TQB2450(1200 mg)静滴(第1天/21天)。主要终点是客观缓解率。次要终点包括无进展生存期、总生存期、疾病控制率和安全性。
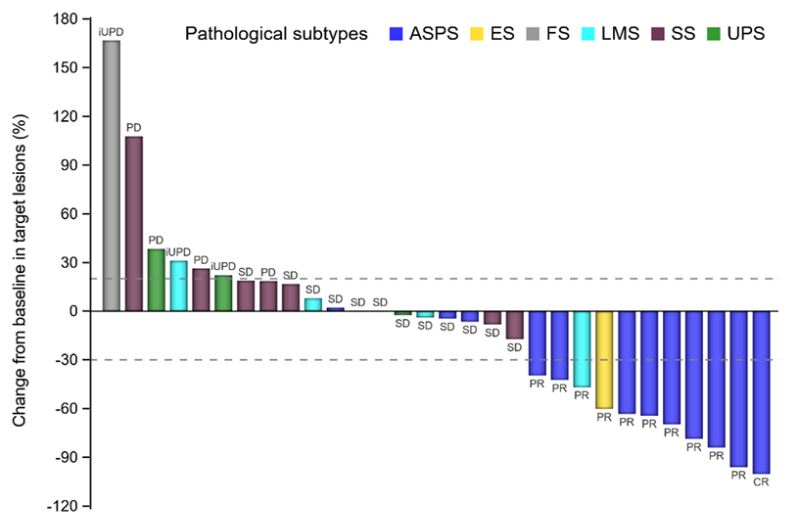
所有患者的治疗反应
2019年1月-2020年6月,共招募了30位患者。客观缓解率为36.67%,疾病控制率为76.67%。中位无进展生存期是7.85个月,中位总生存期未达到。在腺泡状软组织肉瘤患者(n=12)中,客观缓解率为75%,中位无进展生存期是23.06个月。
总受试患者的无进展生存率
最常见的治疗相关不良反应有甲状腺功能减退(76.67%)、高甘油三酯血症(63.33%)、高胆固醇血症(60.00%)和血乳酸脱氢酶升高(53.33%)。
综上所述,该研究结果显示,TQB2450联合安罗替尼在腺泡状软组织肉瘤中的疗效可期,在其他类型肉瘤中也展现出了疗效趋势,而且毒性可控。值得进一步研究验证。
原始出处:
Jiayong Liu; Tian Gao; Zhichao Tan, et al. Phase II study of TQB2450, a novel PD-L1 antibody, in combination with anlotinib in patients with locally advanced or metastatic soft tissue sarcoma. Clin Cancer Res clincanres.0871.2022-3-18 10:13:03.583. https://doi.org/10.1158/1078-0432.CCR-22-0871.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#局部晚期#
45
#软组织肉瘤#与#安罗替尼#
61
#PD-L1#
65
#转移性#
49
#局部#
50
#软组织#
41
学习了,谢谢分享
38