JAMA OHNS:应用临床参数判断小儿OSAS的程度
2014-12-08 zhangjialiang译 MedSci原创
临床中,儿童鼾症可分为单纯性鼾症和小儿阻塞性呼吸睡眠暂停综合征(Obstructive SleepApnea Syndrome,OSAS)两类。单纯性鼾症患儿睡眠过程中不伴有睡眠呼吸暂停,无需手术治疗。小儿OSAS发病峰值年龄2~6岁,可能与淋巴组织增生过旺有关。由于夜间缺氧、C02滞留,干扰脑组织能量代谢,患儿白天多表现为晨起头痛、嗜睡、烦躁、易激惹、注意力不集中,甚至性格、行为异常。30%~5
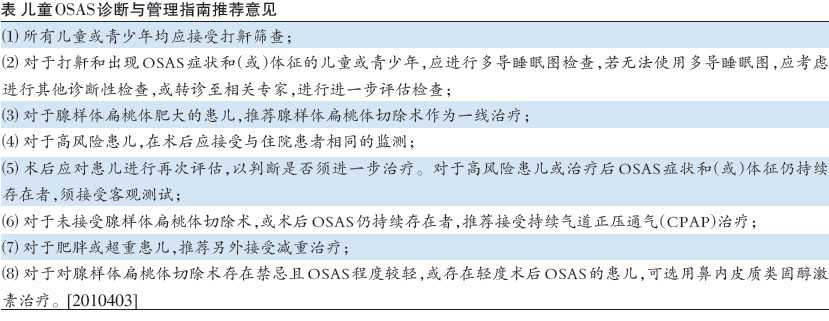
临床中,儿童鼾症可分为单纯性鼾症和小儿阻塞性呼吸睡眠暂停综合征(Obstructive Sleep Apnea Syndrome,OSAS)两类。单纯性鼾症患儿睡眠过程中不伴有睡眠呼吸暂停,无需手术治疗。小儿OSAS发病峰值年龄2~6岁,可能与淋巴组织增生过旺有关。由于夜间缺氧、C02 滞留,干扰脑组织能量代谢,患儿白天多表现为晨起头痛、嗜睡、烦躁、易激惹、注意力不集中,甚至性格、行为异常。30%~50%患儿生长发育不同程度落后于同龄儿,长期上呼吸道阻塞,张口呼吸可影响面部及牙齿发育,甚至出现腺样体面容,如长脸、下颌骨平面较陡、颌后缩,安静时上下唇张开,上唇相对较短。严重的低氧血症、高碳酸血症还会引起心血管并发症,危及患儿生命,如发作频繁或持续时间过长可引起肺动脉高压、右心衰竭及肺心病,缺氧发作时还可引起心动过缓、心律失常、甚至心跳停止、缺氧性晕厥。因此,小儿OSAS具有明确手术指证,而合理选择手术适应症患儿是治疗小儿鼾症的基本原则。 Mitchell博士是西南德克萨斯州大学耳鼻咽喉头颈外科及儿童医学中心的研究人员。她说:“目前尚无公认的判断儿童OSAS的分级,这关乎患儿进行腺样体扁
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#OSAS#
0
仍然需进一步研究
119
#SAS#
35
比较前沿,学习了。
100
#OSA#
29