eLife:T细胞受体基因疗法或可有效改善癌症免疫疗法的安全性
2016-11-12 佚名 生物谷
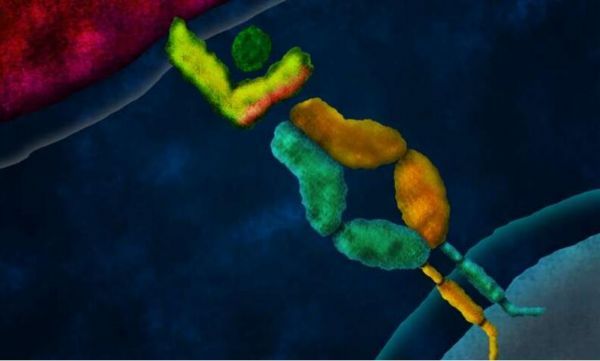
图片来源:medicalxpress.com 人类机体能够产生T细胞来识别并且抵御疾病,每个T细胞在其表面都有着特殊的T细胞受体(TCR),这些受体能够实时监视来自别的细胞呈递的蛋白质小片段,当检测到癌症或感染时,一类T细胞就会同疾病细胞结合并且促进这些细胞被清除,当肿瘤和感染不能够被自然消除时,研究者们就会采用免疫疗法来增强免疫系统的效力。 通过将编码肿瘤特异性TCR的基因插入到患者机体

图片来源:medicalxpress.com
人类机体能够产生T细胞来识别并且抵御疾病,每个T细胞在其表面都有着特殊的T细胞受体(TCR),这些受体能够实时监视来自别的细胞呈递的蛋白质小片段,当检测到癌症或感染时,一类T细胞就会同疾病细胞结合并且促进这些细胞被清除,当肿瘤和感染不能够被自然消除时,研究者们就会采用免疫疗法来增强免疫系统的效力。
通过将编码肿瘤特异性TCR的基因插入到患者机体的T细胞中,研究者就开发出了一类能够靶向作用肿瘤细胞的T细胞,这种方法就称之为TCR基因疗法,当常规的癌症疗法失败时,该疗法就能够带来临床上的成功;然而TCR基因疗法并非没有风险,引入的受体能够同每一个工程化的T细胞表面上固有的受体混杂在一起,从而诱发部分细胞对健康细胞进行攻击,而本文中来自加州理工学院的研究人员就开发出了一种特殊技术来抑制上述问题的发生,同时还能够增加TCR基因疗法的安全性。
相关研究刊登于国际杂志eLife上;这种新技术名为功能区切换技术(domain swapping),研究者指出,每个T细胞表面的TCR的特异性都来自两个蛋白质链的配对,也就是α链和β链,每个链都有着恒定域结构和可变域结构,正常情况下,每个T细胞都会编码一条α链和一条β链,这两条链配对就会形成单个TCR,在TCR基因疗法中,编码肿瘤反应性TCR基因的引入则会导致T细胞表达两条α链和两条β链,这样就会形成四种可能性的组合方式,而这种非生理学的状况就会引发自身免疫的风险。
研究者Michael Bethune说道,随着T细胞产生,免疫系统就会让其“试镜”,从而消除那些对自身健康细胞产生反应的T细胞,最终留下来能够识别疾病细胞的T细胞。然而在能够表达TCR的工程化T细胞中,引入的蛋白链能够同固有的链进行错误配对,最终使得TCRs具有不可预测的特异性,免疫系统并不会对这些错误配对的TCRs进行“试镜”,从而就会导致某些免疫细胞靶向作用健康细胞引发自身免疫反应。在注射了TCR工程化T细胞的小鼠机体中,有90%的小鼠都会患上自身免疫疾病。
研究者Bethune说道,功能区切换链和固有链之间的错误配对会导致TCR缺失其复合物功能性装配所需的结构域;这项研究中研究者重点关注了功能区切换所带来的TCR基因疗法的安全性,但研究者认为,对不同方法进行结合或许就能够改善基因疗法的安全性,当然后期他们还需要进行更为深入的探索才能够深入阐明新型TCR基因疗法的作用效果和安全性。
原始出处
Michael T Bethune Marvin H Gee Mario Bunse Mark S Lee Eric H Gschweng Meghana S Pagadala Jing Zhou Donghui Cheng James R Heath Donald B Kohn Michael S Kuhns Wolfgang Uckert David Baltimore.Domain-swapped T cell receptors improve the safety of TCR gene therapy.eLife.2016
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#eLife#
28
#Life#
24
学习…,赞一下!
42
学习一下,赞一下!
56
#T细胞受体#
0