JCEM:骨髓脂肪是骨强度的独立预测因子
2013-05-06 JCEM dxy
机械负荷的增加可以促进骨髓间充质干细胞优先向成骨细胞分化,但在人类,长期骨骼力量强化锻炼是否能减少骨髓脂肪仍不清楚。为了验证作为判断骨髓脂肪过多的骨髓密度(MaD),在年龄女性运动员负荷史和骨强度对比中是否不同,以及骨髓密度在胫骨负重中是否是骨强度的独立预测因子,来自澳大利亚迪肯大学的Timo Rantalainen教授及其团队进行了一项研究,该研究发现在年龄女性运动员,胫骨MaD与负荷史有关,并
机械负荷的增加可以促进骨髓间充质干细胞优先向成骨细胞分化,但在人类,长期骨骼力量强化锻炼是否能减少骨髓脂肪仍不清楚。为了验证作为判断骨髓脂肪过多的骨髓密度(MaD),在年龄女性运动员负荷史和骨强度对比中是否不同,以及骨髓密度在胫骨负重中是否是骨强度的独立预测因子,来自澳大利亚迪肯大学的Timo Rantalainen教授及其团队进行了一项研究,该研究发现在年龄女性运动员,胫骨MaD与负荷史有关,并是胫骨强度的独立预测因子。该研究结果在线发表在2013年4月24日的美国《临床内分泌代谢杂志》(The Journal of Clinical Endocrinology & Metabolism)上。
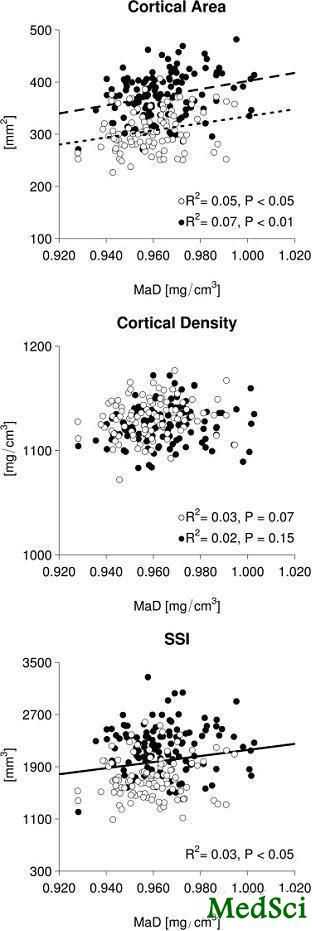
该研究,在179例女性运动员包括冲击和非冲击负荷运动和41例年龄17–40岁的对照者中,使用外周定量CT评估胫骨中段MaD、皮质骨面积(CoA)、总面积、骨髓面积、扭伤力指数(SSI)、以及皮质骨体积骨密度(vBMD)(总的、皮质骨内、皮质骨中间和皮质骨周围)。
该研究结果表明,如同以前报道的一样,冲击组CoA、总面积和SSI比对照组高16%至24%(所有P<0.001),并比非冲击组高12%至18%(所有P<0.001)。同样,冲击组MaD比非冲击组和对照组高0.5%(两个P<0.05)。校正年龄、骨长度、负荷组别、骨髓面积、肌肉横断面积和脂肪百分比后,在所有女性组合中,进一步的回归分析显示胫骨中段MaD与SSI、CoA、皮质骨内vBMD和皮质骨周围vBMD显著相关(P<0.05)。
该研究发现,在年轻女性运动员,胫骨MaD与负荷史有关,并是胫骨强度的独立预测因子。这些发现提示锻炼可能通过介导骨髓脂肪减少,从而增加成骨细胞发生,诱导骨强度增加。
与骨相关的拓展阅读:
- JCEM:骨钙蛋白与骨骼肌胰岛素敏感性有关
- JBJS:股骨转子部骨折的内固定疗效——髓内钉优于滑动髋螺钉吗?
- 三男子醉酒动粗拳打医护人员 一护士额骨骨折
- JCEM:溃疡性结肠炎患者有更高的低骨矿密度患病率
- 东亚地区锁骨肿瘤回顾性荟萃分析 更多信息请点击:有关骨更多资讯

Differential Effects of Exercise on Tibial Shaft Marrow Density
Context
Increased mechanical loading can promote the preferential differentiation of bone marrow mesenchymal stem cells to osteoblastogenesis, but it is not known whether long-term bone strength-enhancing exercise in humans can reduce marrow adiposity.
Objective
Our objective was to examine whether bone marrow density (MaD), as an estimate of marrow adiposity 1) differs between young female athletes with contrasting loading histories and bone strengths and 2) is an independent predictor of bone strength at the weight-bearing tibia.
Design
Mid-tibial MaD, cortical area (CoA), total area, medullary area, strength strain index (SSI), and cortical volumetric bone mineral density (vBMD) (total, endocortical, midcortical, and pericortical) was assessed using peripheral quantitative computed tomography in 179 female athletes involved in both impact and nonimpact loading sports and 41 controls aged 17-40 years.
Results
As we have previously reported CoA, total area, and SSI were 16% to 24% greater in the impact group compared with the controls (all P < .001) and 12% to 18% greater than in the nonimpact group (all P < .001). The impact group also had 0.5% higher MaD than the nonimpact and control groups (both P < .05). Regression analysis further showed that midtibial MaD was significantly associated with SSI, CoA, endocortical vBMD, and pericortical vBMD (P < .05) in all women combined, after adjusting for age, bone length, loading groups, medullary area, muscle cross-sectional area, and percent fat.
Conclusion
In young female athletes, tibial bone MaD was associated with loading history and was an independent predictor of tibial bone strength. These findings suggest that an exercise-induced increase in bone strength may be mediated via reduced bone marrow adiposity and consequently increased osteoblastogenesis.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#JCE#
27
#骨强度#
32
#JCEM#
39
#预测因子#
37