瞄准癌细胞的芯片:麻省总医院和强生合作将其商业化
2014-03-07 苏珊·杨(Susan Young) 科技评论
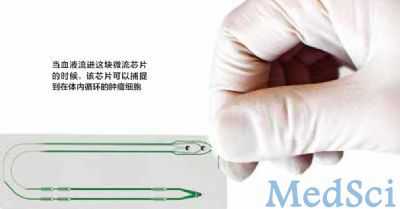
在不远的将来,肿瘤学家也许可以用手指大小、带有微小管道的塑料芯片从病人的血液中提取十几个癌细胞。这些细胞是循环肿瘤细胞,可以在被提取后接受筛选,找到让肿瘤学家能够选择最佳标靶药物的遗传变异。持续地采样可以让医生检测某种治疗方法是否有效,并让他们决定是否随着疾病的进化,添加或替换某种药物。 有数十家公司正在这个市场中竞争。据估计,这一市场在未来几年会达到 79 亿美元。强生
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#商业#
32
#总医院#
31
#癌细胞#
31
#强生#
22
#芯片#
27
#商业化#
30