AP&T: 高压氧疗法治疗克罗恩病20例肛周瘘管疗效分析
2021-02-19 MedSci原创 MedSci原创
肛周瘘是克罗恩病的常见并发症,大约三分之二的克罗恩病人在病程中至少发生一次瘘管。瘘管自发性闭合很少见,大多数患者需要医疗和/或手术干预。
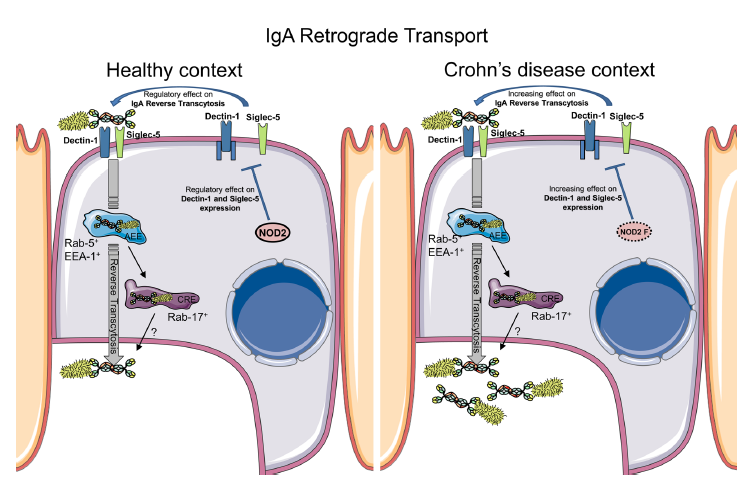
肛周瘘是克罗恩病的常见并发症,大约三分之二的克罗恩病人在病程中至少发生一次瘘管。瘘管自发性闭合很少见,大多数患者需要医疗和/或手术干预。由抗肿瘤坏死因子为主的疗法成功率约为40%。不幸的是,在高达50%的患者中,瘘确会在2年内复发。间质干细胞的使用在某些复杂瘘管病例中是一种新的治疗方式。最近的一项研究表明,在瘘管周围注入干细胞来封闭内部开口可在第24周使50%的患者实现临床和放射学愈合。高压氧治疗已被建议作为IBD患者的潜在辅助治疗方法。高压氧疗法是指在高于正常大气压的条件下呼吸100%的氧气:通常为202-253千帕斯卡(相当于2.0-2.5大气压)。本项研究旨在评估高压氧在克罗恩病伴难治性肛周瘘管患者中的有效性,安全性和可行性。

研究人员在阿姆斯特丹的医疗诊所招募了20名连续的克罗恩病肛周瘘管患者,所有患者为包括高位肛周瘘的,常规治疗失败超过6个月的克罗恩病患者。排除标准为存在造口,直肠阴道瘘和近期治疗方案的改变。所有患者在接受了40次高压氧治疗后,并在第16周评估了预后指标。
研究结果发现在第16周,克罗恩病患者的肛周疾病活动指数从7.5(95%CI 6-9)降至4(95%CI 3-6,P <0.001),改良的van Assche指数的中位数评分从9.2(95%CI 7.3-11.2)到7.3(95%CI 6.9-9.7,P = 0.004)。在13/20例患者中(65%)观察到的肛周疾病活动指数得分≤4(代表非活动性肛周疾病)。通过瘘管引流评估评估的十二名患者表现出临床反应(60%)和(20%)临床缓解。所有患者的C反应蛋白从4.2 mg / mL(95%CI 1.6-8)降至2.2(95%CI 0.9-4.3,P= 0.003),粪便钙卫蛋白的中位数从399 µg / g降低至31ug/g, P = 0.001)。
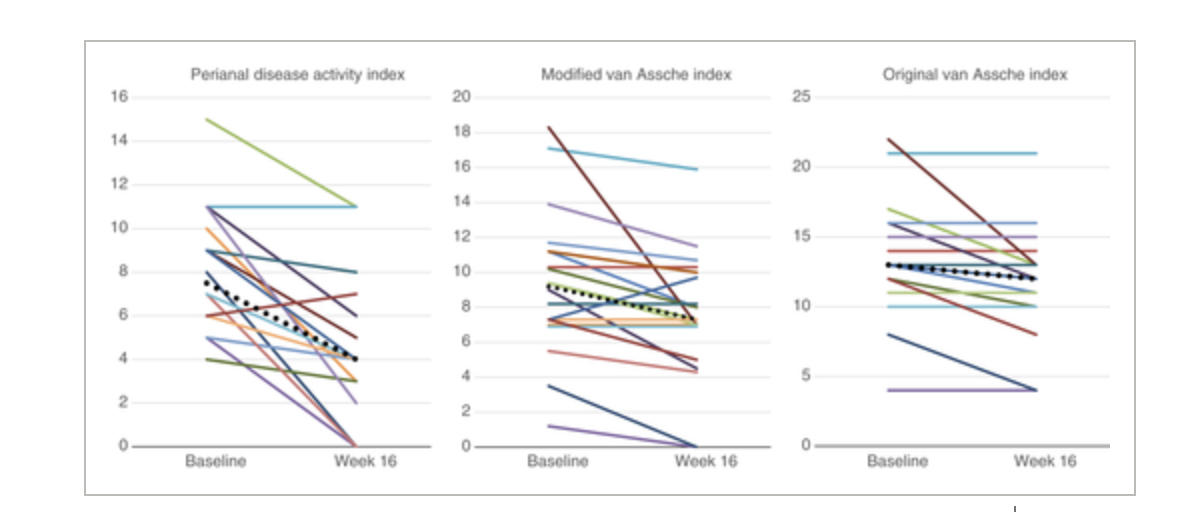
通过本项研究作者发现高压氧治疗后患有难治性肛周瘘管的克罗恩病患者在临床,放射学和生化方面均有显着改善。
原始出处:
Corine A. Lansdorp. Et al. Hyperbaric oxygen therapy for the treatment of perianal fistulas in 20 patients with Crohn’s disease.Alimentary Pharmacology & Therapeutics.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#疗效分析#
33
#肛周瘘管#
33
#肛周瘘#
38
#高压氧#
42
#氧疗#
53
谢谢梅斯提供这么好的信息,学到很多
48
可以可以
66