AACR 2022:NK细胞及双特异性抗体AFM13复合物持续诱导淋巴瘤缓解
2022-04-12 Allan MedSci原创
在 19 名可评估患者中,17 名对治疗有反应,总缓解率 (ORR) 为 89%。
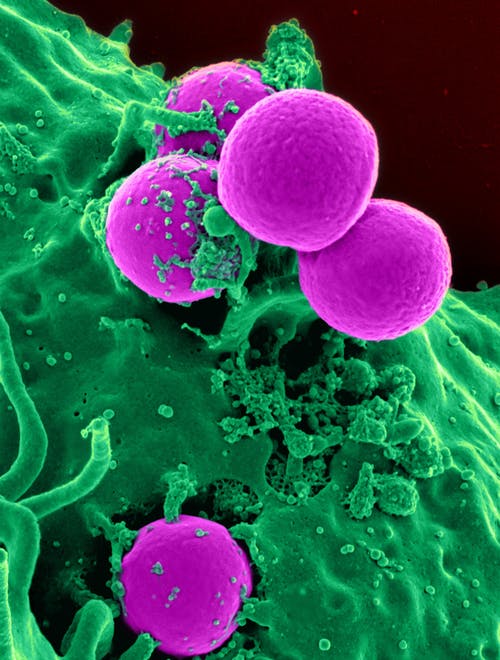
周日在美国癌症研究协会 (AACR) 年会上公布的 I/II 期研究结果显示,双特异性抗体 AFM13 与NK细胞的复合物继续诱导复发性 CD30+ 淋巴瘤患者的缓解。介绍该研究的 Yago Nieto 说:“我们的初步结果表明,在这一经过大量先前治疗的患者群体中,复合物的活性和耐受性是有希望的,值得进一步研究”。
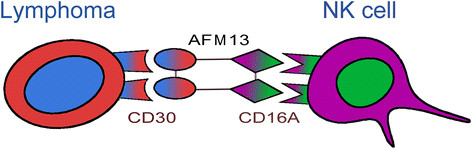
AFM13 能够靶向 CD16A 和 CD30,与脐血来源的同种异体 NK 细胞预复合后治疗 CD30+ 复发或难治性霍奇金淋巴瘤和非霍奇金淋巴瘤患者,这些患者的中位先前治疗线为 7。
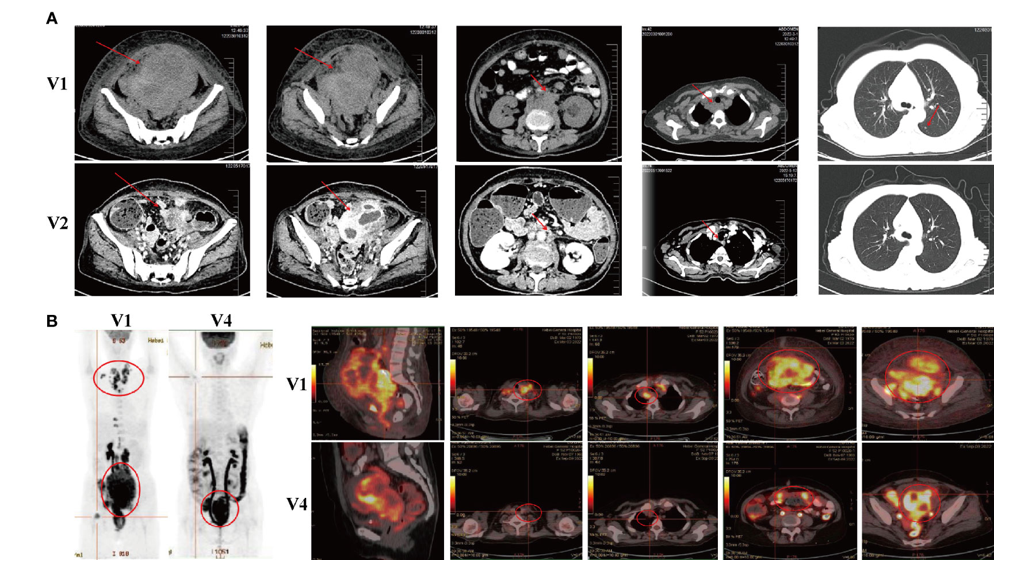
在经历免疫细胞清扫后,受试者接受了两个周期的 AFM13-NK 细胞复合物治疗,最高为 1 亿个细胞/kg,给予 13 名患者,并被选为 II 期评估的剂量。随后还进行了每周 3 次 AFM13 单一疗法的输注,并在第 28 天评估反应。
在 19 名可评估患者中,17 名对治疗有反应,总缓解率 (ORR) 为 89%。其中包括以推荐的 II 期剂量水平治疗的所有 13 名患者,其中有 8 名(62%)完全缓解(CR)和 5 名患者部分缓解(PR)。在 8 例 CR 中,7 例在中位 6.5 个月的随访后仍处于完全缓解状态,其中 2 例在 10 个月后仍保持完全缓解,2 例接受了自体干细胞移植。研究人员表示,在所有剂量水平上,中位随访 11 个月后,无进展生存率和总生存率分别为 53% 和 79%。
同时,该疗法耐受性良好,没有出现细胞因子释放综合征、免疫效应细胞相关神经毒性或移植物抗宿主病的病例。
原始出处:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#特异性#
67
#复合物#
45
#NK细胞#
58
#ACR#
56
#特异性抗体#
32
#AACR#
34