Blood:阻断PD-1通路可能阻止慢性淋巴细胞性白血病向急性淋巴细胞性白血病转化
2017-06-30 MedSci MedSci原创
使用PD-1阻断抗体能够安全有效的抑制慢性淋巴细胞性白血病病人发生Richter转化,如果未来这一结果能够被进一步的验证,则有可能可以改变慢性淋巴细胞性白血病病人的治疗方式。
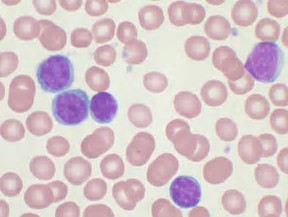
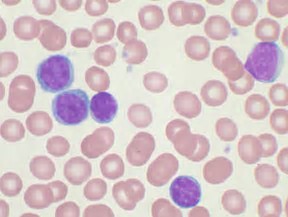
慢性淋巴细胞性白血病(chronic lymphocytic leukemia, CLL)患者在早期使用依鲁替尼(ibrutinib,布鲁顿酪氨酸激酶抑制剂)后,可能会发生Richter李希特转化(Richter transformation,RT)由慢性淋巴细胞性白血病转化为急性的淋巴细胞白血病,导致存活时间约4个月。临床前研究表明,程序性死亡1(PD-1)信号通路对于抑制慢性淋巴细胞性白血病中激活免疫反应至关重要。
在最新的一期Blood杂志中,Wei Ding及其同事报导了一项他们执行的使用Pembrolizumab(anti-PD-1靶向单克隆阻断抗体)抑制慢性淋巴细胞性白血病向急性淋巴细胞性白血病转化的2期临床试验。
该项研究旨在研究和测试在复发和转化的慢性淋巴细胞性白血病病人中,以每3周200mg的剂量测试pembrolizumab的功效和安全性。在入选的25例患者,其中包括16例为复发性慢性淋巴细胞性白血病病人和9例发生Richter转化(全部证实为转化为弥漫性大细胞淋巴瘤)的患者。其中,60%接受曾接受依鲁替尼的治疗。在9例发生Richter转化的患者中有4例(44%),16例慢性淋巴细胞性白血病患者中有0例观察到依鲁替尼的治疗客观治疗反应。经过11个月的中位随访时间后,发生Richter转化的组别中位生存期为10.7个月。 15例(60%)患者报告了发生了与治疗相关3级或以上不良事件,但是这些时间都在可控范围内。
总之,使用PD-1阻断抗体能够安全有效的抑制慢性淋巴细胞性白血病病人发生Richter转化,如果未来这一结果能够被进一步的验证,则有可能可以改变慢性淋巴细胞性白血病病人的治疗方式。
原始出处:
Wei Ding et al. Pembrolizumab in patients with CLL and Richter transformation or with relapsed CLL. Blood 2017 129:3419-3427; doi: https://doi.org/10.1182/blood-2017-02-765685
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#阻断#
33
#细胞性#
26
阻断通路可能阻止l慢性白血病。
62
#淋巴细胞#
28
#慢性淋巴细胞性白血病#
0
学习,谢谢分享
66
谢谢分享,学习了
61
学习谢谢分享
58
谢谢了,学习
61
学习了谢谢分享
20