Nature Nanotechnology:喝杯“纳米汁”,看清你的肠道
2014-07-08 佚名 科学人
小肠身处人体肠道深处,一直以来,想要给它做个全面检查都不太容易。X射线、磁共振以及超声波成像能够提供小肠图像,但这些方法都各有缺陷。不过,医生们马上就要有个新的好帮手了。 布法罗大学的研究人员正在研发一种全新的非侵入式成像技术:将纳米粒子悬浮液制成“纳米汁”让病人服下,等到“纳米汁”抵达小肠时,医生们即可用一束对人体无害的激光照射小肠内的纳米粒子,从而获得实时的器官影像。该研究的相关论文于近日发表
小肠身处人体肠道深处,一直以来,想要给它做个全面检查都不太容易。X射线、磁共振以及超声波成像能够提供小肠图像,但这些方法都各有缺陷。不过,医生们马上就要有个新的好帮手了。
布法罗大学的研究人员正在研发一种全新的非侵入式成像技术:将纳米粒子悬浮液制成“纳米汁”让病人服下,等到“纳米汁”抵达小肠时,医生们即可用一束对人体无害的激光照射小肠内的纳米粒子,从而获得实时的器官影像。该研究的相关论文于近日发表在《自然•纳米技术》期刊上。根据论文描述,该技术能够帮助医生更好地识别、理解以及治疗肠道疾病。
“传统的成像方法可以显示小肠及内部的阻塞物,但是这项新技术能够让你看到小肠实时的运作情况,”论文的通讯作者乔纳森•洛弗尔(Jonathan Lovell)博士说到,他是布法罗大学的一名医药工程助理教授。“更好的成像技术能够提升我们对疾病的理解,并帮助医生为患者提供更有效的治疗。”
小肠位处胃与大肠之间,这里是食物消化吸收过程的主要发生地。它也是肠易激综合征、乳糜泻、克罗恩病等消化系统疾病的发病位置。
在小肠影像检查的通常流程下,医生会让患者喝下一种名叫“钡餐”(硫酸钡)的稠密的白色液体,并进行X射线检查,或是利用磁共振或超声波对小肠进行成像。但这些方法各自都有一些缺陷,譬如,X射线在安全方面存在一定局限性,磁共振成像的普及性较差,而超声波成像的对比度又有不足。
而且,要想看到器官实时的运动情况,譬如小肠在推动食物前进时因肌肉收缩引起的蠕动,上述三种传统方法都不怎么有效。小肠运动异常可能与之前提到的几种肠胃疾病有关,同时也可能是甲状腺疾病、糖尿病和帕金森氏病的副产物。
洛弗尔和他的团队在研究中使用了一类名叫萘酞菁化合物(naphthalcyanines)的染料。这种小分子能够吸收很大一部分的近红外光,而近红外光正是生物造影剂的理想光谱范围。但萘酞菁化合物在体内并不怎么好用,因为它们不容易在液体中分散,进入小肠后也会被吸收进入血管,而不能保留在肠道内。
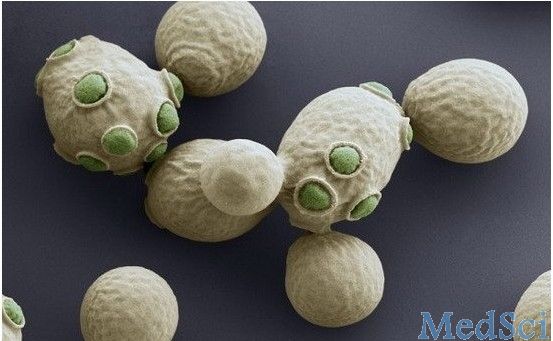
为了解决这些问题,研究人员制作了一种名叫“nanonaps”的纳米粒子,将染料分子包裹其中。与染料分子本身不一样的是,这种纳米粒子容易在液体中分散,并且能安全通过肠道,避免染料被吸收。
在实验中,研究人员给小鼠口服了这种“纳米汁”。 随后,他们使用光声成像技术(photoacoustic tomography,PAT)获得了较传统方法细节更为丰富的小肠实时图像。PAT是一种新兴的成像技术,它利用光声效应的原理,通过脉冲激光照射产生超声波,再利用体表的超声波测试仪接收信号并重建图像。
研究人员正在计划进一步改良这项技术,使之更适用于人体,并将成像对象从小肠扩展至其他胃肠区域。
原始出处:
Yumiao Zhang, Mansik Jeon, Laurie J. Rich, Hao Hong, Jumin Geng, Yin Zhang, Sixiang Shi, Todd E. Barnhart, Paschalis Alexandridis, Jan D. Huizinga, Mukund Seshadri, Weibo Cai, Chulhong Kim& Jonathan F. Lovell. Non-invasive multimodal functional imaging of the intestine with frozen micellar naphthalocyanines. Nature Nanotechnology, 06 July 2014;
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#TEC#
37
#Technology#
47
#Nat#
35
第一作者还是中国人 天津大学 南开大学双学位 来自于黑龙江省 Yumiao Zhang 张育淼
79
研究胃肠功能障碍的利器
137
研究胃肠功能障碍的利器
105